Glaucoma is a leading cause of irreversible blindness worldwide. Find out from Dr Low Jin Rong, Consultant, Glaucoma Department at Singapore National Eye Centre (SNEC) about the risk factors, symptoms and treatment for this condition.
In Singapore, glaucoma accounts for 34 per cent of blindness.
Often termed the 'Silent Thief of Sight', glaucoma is hardly noticeable in its early stages as patients usually do not show any symptoms.
It is only during the advanced stages, when the visual loss is profound, that patients notice a significant impact on their lives.
Glaucoma is an eye condition that damages the eye's optic nerve and usually develops as a consequence of high pressure within the eye. It is characterised by a progressive loss of vision due to damage to the optic nerve which carries visual information from the eye to the brain.
Although the condition cannot be cured, in most cases, blindness from glaucoma is preventable if the disease is detected early and can be successfully controlled with a combination of either eyedrops, laser or surgery.
Thus, early detection is crucial in preventing vision loss or slowing the condition's progression, which can be done through going for regular eye check-ups and knowing your family's history of glaucoma.
For more on what you can do to minimise risk of glaucoma, check out this article.
Don't get blindsided by glaucoma, help shed light on the topic by asking Dr Low about the causes, symptoms and treatment options for this condition. This Q&A is only for a limited time so submit your question now!
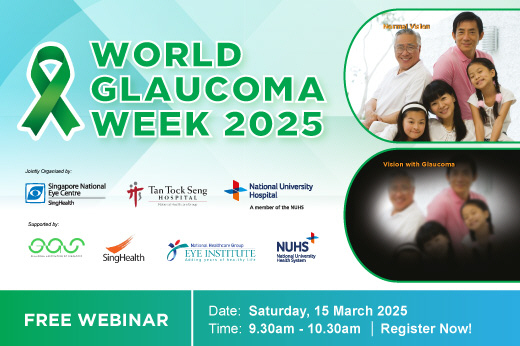
Join us for World Glaucoma Week 2025 webinar, taking place on 15 Mar 2025 (Sat) from 9.30am to 12 noon. This webinar is available in English and Mandarin. To register for this webinar and for more details, click here. |
About Dr Low Jin Rong
Dr Low Jin Rong is a Consultant in the Glaucoma Department at SNEC. He is actively involved in ophthalmology training of local and overseas clinical fellows, residents, medical students, nurses and allied health professionals, and was awarded the NUS Junior Doctor Teaching Award (2018), the SNEC Outstanding Educator Award (2021) and the SingHealth Residency - Outstanding Faculty Award (2023) for his contributions to medical education.
Dr Low is also active in ophthalmic research and has published numerous scientific papers in respected peer-reviewed medical journals and presented his research work at international and local scientific conferences.
His research interests include the value-driven outcomes of minimally invasive glaucoma surgery (MIGS), and how glaucoma disease and treatments affect patients’ quality of life. He is the Clinical Lead of MIGS in SNEC and has written guidelines on its use in patients with glaucoma.
Questions and answers on managing glaucoma
1. Question by Wan Tiau
Dear Dr Low Jin Rong,
Is it true that it is helpful to take Vitamin D for glaucoma patients, in order to slow down the deterioration rate?
Answer by Dr Low Jin Rong
Dear Wan Tiau,
While there is some evidence to suggest a link between vitamin D deficiency and increased glaucoma severity, the overall scientific consensus is not definitive.
Further research is necessary to establish whether vitamin D supplementation can effectively slow down glaucoma progression.
2. Question by Patrina
Dear Dr Low,
May I know if TCM can treat or cure glaucoma? Thank you.
Answer by Dr Low Jin Rong
Dear Patrina,
Traditional Chinese Medicine (TCM) offers various approaches that may complement conventional glaucoma treatment. For example, Ginkgo Biloba, known for enhancing blood circulation, has been studied for its potential benefits in glaucoma management.
However, it is important to note that TCM should not replace standard medical treatment for glaucoma. Patient interested in incorporating TCM into their glaucoma management plan should consult with their ophthalmologist and a qualified TCM practitioner to ensure a safe and coordinated approach.
In additional, glaucoma currently cannot be cured but it can be managed to slow down its worsening and to prevent further vision loss. The damage to the optic nerve caused by glaucoma is irreversible, so early detection and treatment are crucial.
3. Question by Lee Tan
Dear Dr,
How often and where do we go for regular eye check up? Is there government support in this respect in terms of cost?
Answer by Dr Low Jin Rong
Dear Lee Tan,
According to the American Academy of Ophthalmology (AAO) recommendations, a comprehensive eye examination, including glaucoma screening, should be performed at the following intervals for individuals without known risk factors:
Ages 40 to 54: Every 2 to 4 years
Ages 55 to 65: Every 1 to 3 years
Ages 65 and older: Every 1 to 2 years
For individuals at higher risk, such as having a family history of glaucoma, early and more frequent screenings are recommended. Your ophthalmologist will advise you on the interval of follow up based on your screening results. If you have any eye or visual symptoms, you are recommended to have your eyes checked by an ophthalmologist.
There are various government subsidies and programmes available. You may visit the official HealthHub website for further details.
4. Question by Carol
Hi Dr,
I just turned 60 years old. I recently was told I have narrow drainage angles. Does that mean I will eventually have glaucoma? What should I do? Thank you for your advice.
Answer by Dr Low Jin Rong
Dear Carol,
Having narrow drainage angles increases your risk of developing angle-closure glaucoma.
However, not everyone with narrow drainage angles will develop glaucoma. The key concern is that fluid drainage in your eye can become blocked, leading to increased eye pressure, which can damage the optic nerve.
You should have regular eye examination by your ophthalmologist to monitor your eye angles, eye pressure and optic nerve. If you experience sudden eye pain, headache, blurry vision, haloes around lights, nausea or vomiting, please seek emergency medical attention, as these symptoms could indicate a sudden angle-closure attack of your eyes, which requires urgent treatment.
Treatment options for narrow drainage angles include:
Laser Peripheral Iridotomy, which creates a small hole in the iris to allow fluid drainage and reduce pressure buildup, and
Cataract Surgery, which removes the cataract, deepens the drainage angle and lower the risk of glaucoma.
You may discuss with your ophthalmologist on the most appropriate treatment plan that is personalised to your condition.
5. Question by Wei Yuen
Hello Doctor,
Since there are no obvious signs and symptoms of glaucoma at the early stages. Where and how do we have our eyes checked - at normal optical shops???
It would be helpful if there’s a scheme for a certain age (maybe 60 and above - I am not sure which is the most vulnerable age group) to have their eyes checked at a subsidised fee just like the other chronic diseases.
Answer by Dr Low Jin Rong
Dear Wai Yuen,
Given that glaucoma often presents without symptoms in its early stages, regular eye examinations are essential for early detection and management.
Individuals can access eye screening services through various avenues such as public healthcare institutions, private eye clinics, and certain general practitioner (GP) clinics and optometry shops which are equipped to perform basic eye screenings and can refer individuals to eye specialists if necessary. SNEC and other eye care institutions also regularly hold public eye screening events.
To receive subsidised care at public Specialist Outpatient Clinics (Ophthalmology), individuals may obtain a referral from a polyclinic or Community Health Assist Scheme (CHAS) GP clinic.
6. Question by Richard
Hi Dr Low,
I am a male, 77 years old. Chinese. I have had glaucoma in both eyes since 2006. About 18 years.
I have been shorted-sighted since primary school days.
I also had 2 failed drainage implants 9 years ago (scar tissue) and went through subsequent cyclodiode laser treatments in both eyes after that. Had pulse diode treatment last 2-3 years which helped stabilise IOP.
I use xalatan and azarga eyedrops everyday to treat my glaucoma condition.
In recent 2-3 months, with newly prescribed distance glasses and reading glasses, my vision has been erratic: sometimes clear, sometimes blurry.
More so with reading glasses than distance glasses.
Reading glasses vision is better with backlit devices.
I experience on/off, clear and blurry vision reading a book (in normal daylight) with printed pages.
What is happening to my vision that I now struggle to see clearly?
By the way at 77, I have had hypothyroidism for around 15 years too and take thyroxine medication every day.
Please help! Thank you for your advice.
Answer by Dr Low Jin Rong
Dear Richard,
Thanks for sharing your past ocular history and current treatment regime. The symptoms of intermittent blurring of vision which you have described may be related to dryness of your eyes.
I will suggest an evaluation of your eyes by your ophthalmologist to check for poor ocular surface. This may necessitate use of ophthalmic lubricants and/or consider a change of your glaucoma eye drops to preservative-free forms.
7. Question by Caroline
Good day Dr Low.
I'm a senior, recently had new short- and long-sighted glasses made and discovered I have amblyopia, left eye 250° (right 50°, no change) which used to be 100°. I have an appointment at the end of Apr.
Meanwhile I'm switching and wearing the new glasses constantly.
I exercise daily, watch what I eat and take a statin for cholesterol which is under control.
Am I susceptible to developing glaucoma? Anything else I can do about the left lazy eye? Thank you.
Answer by Dr Low Jin Rong
Dear Caroline,
Thanks for sharing your medical conditions. Increasing age and short-sightedness (myopia) are risk factors for glaucoma.
I will advise you to keep to your eye appointment. Your ophthalmologist will perform a comprehensive eye evaluation to screen for glaucoma and to ascertain your diagnosis of lazy eye (amblyopia).
Customised optical corrections such as glasses may help to maximize the vision in your amblyopic eye.
8. Question by Jamie
Dear Dr Low, I have the following questions:
Personal risk assessment
a) Given that two of my siblings (2 out of 5) have glaucoma, what is my estimated risk of developing it?
b) Are there specific genetic factors that could explain why my siblings developed glaucoma despite no known family history?
c) Should I consider genetic testing for glaucoma-related mutations?
d) Do my other siblings who don’t have glaucoma still have a higher risk, and should they also be screened more frequently?
Screening and diagnosis
a) How often should I have my eyes examined given my family situation?
b) Are there early warning signs I should be aware of, even if my eye pressure is normal?
c) Can glaucoma be detected before symptoms appear, and what are the chances of early treatment preventing vision loss?
Prevention and lifestyle
a) Are there any lifestyle changes or habits that can reduce my risk of developing glaucoma
b) Does diet, exercise, or sleep affect glaucoma risk?
c) Are there specific medications or medical conditions that could increase my risk of glaucoma?
d) Does prolonged screen time or excessive eye strain have any impact on glaucoma development?
Treatment and management
a) If I am diagnosed with early-stage glaucoma, what treatment options are available?
b) Are there any new advancements in glaucoma treatment or prevention that I should be aware of?
c) How does treatment differ depending on the type of glaucoma?
d) If I develop glaucoma, how likely is it to progress to vision loss despite treatment?
Family considerations
a) Should my child (or future children) be monitored for glaucoma at an early age?
b) Does the type of glaucoma my siblings have impact my risk differently?
c) Could recurring eye inflammation (as seen in my siblings) be an underlying risk factor for glaucoma in my case?
Final questions
a) Given my family history, is a yearly check-up without seeing a doctor enough, or should I request more frequent monitoring?
b) Should I be seeing a glaucoma specialist instead of just undergoing routine tests?
c) If my eye pressure is normal, does that mean I am safe, or can glaucoma develop despite normal pressure?
d) Would it be beneficial for me to have more comprehensive testing, such as gonioscopy or nerve fiber layer analysis?
e) If early signs of glaucoma are detected, how quickly should I start treatment to prevent vision loss?
f) Is there a possibility of normal-tension glaucoma in my case, given my family history?
Thank you for taking the time to answer my questions.
Answer by Dr Low Jin Rong
Dear Jamie,
Thanks for your in-depth questions regarding glaucoma and its relation to your family history. Here’s a comprehensive response to help you address these concerns:
Personal risk assessment
a) Your risk of developing glaucoma is around 4-6 times higher than the general population, particularly because two of your siblings have it. While the exact risk depends on various factors (age, ethnicity, other health conditions), having close family members with glaucoma increases your risk.
b) Yes, genetic factors can play a significant role in the development of glaucoma, even in the absence of a strong family history. Certain genetic mutations have been identified in people with glaucoma, and some forms of the disease (e.g., primary open-angle glaucoma) may have a genetic component that doesn’t always follow typical inheritance patterns. Even if there isn't an obvious family history, these mutations could still play a part.
c) Genetic testing may be worth considering, particularly if you have a strong family history of glaucoma. It can help identify potential genetic predispositions and could provide you with more information to manage your eye health proactively. However, not all types of glaucoma have well-established genetic markers.
d) Yes, your other siblings still have a higher risk of developing glaucoma, given the family history. It's advisable for them to undergo regular eye exams, especially as they age, as glaucoma can develop without symptoms in its early stages.
Screening and diagnosis
a) Given your family history, you should likely have a comprehensive eye exam at least once a year. This should include measurements of intraocular pressure, a visual field test, and a thorough examination of the optic nerve. If you have additional risk factors (e.g., high blood pressure or being over 40), more frequent monitoring might be necessary.
b) Yes, glaucoma can develop even with normal intraocular pressure. Early warning signs include gradual loss of peripheral vision, difficulty seeing in low light, and in some cases, seeing halos around lights. However, it often progresses slowly without noticeable symptoms until later stages, making regular screening critical.
c) Yes, glaucoma can often be detected early through regular eye exams, even before symptoms appear. Early detection significantly improves the chances of preventing vision loss, as treatment can slow the progression of the disease, especially in its early stages.
Prevention and lifestyle
a) While some factors, such as age and family history, can’t be changed, maintaining a healthy lifestyle can help. This includes eating a balanced diet, avoiding smoking, managing stress, and protecting your eyes from injury. Regular exercise can also help lower intraocular pressure.
b) Yes, regular exercise, such as aerobic activity, can lower intraocular pressure and may reduce glaucoma risk. A diet rich in antioxidants (found in fruits and vegetables) is also beneficial. Poor sleep and sleep apnoea have been linked to higher glaucoma risk, so managing sleep quality is important as well.
c) Certain medications, particularly corticosteroids (used to treat inflammation or other conditions), can increase the risk of glaucoma. Other conditions, like diabetes, hypertension, and high myopia (short-sightedness), can also increase the likelihood of developing glaucoma.
d) There is no strong evidence to suggest that excessive screen time or eye strain directly increases glaucoma risk. However, prolonged screen use can cause eye fatigue and strain, so it's important to take regular breaks to reduce discomfort.
Treatment and management
a) Treatment typically involves medications, such as eye drops, or laser therapy, to lower intraocular pressure. If medication and laser are not effective, surgery may be necessary. Early-stage glaucoma can often be managed effectively with regular treatment.
b) Recent advancements include new classes of eye drops with fewer side effects and more effective pressure-lowering properties. Additionally, minimally invasive glaucoma surgeries (MIGS) are a promising option for patients with various severity of glaucoma.
c) Treatment varies depending on the type of glaucoma. For open-angle glaucoma, medication (eye drops) is typically the first line of treatment. For angle-closure glaucoma, laser surgery or other procedures may be necessary to widen the drainage angle.
d) With proper treatment, the progression of glaucoma can usually be slowed or halted, but it varies from person to person. Early detection and adherence to treatment are crucial for preventing significant vision loss.
Family considerations
a) While glaucoma is more common in adults, early screening may be considered if there is a strong family history. Your child’s risk is higher if you or your siblings have glaucoma.
b) Yes, if your siblings have a specific type of glaucoma (such as angle-closure glaucoma or normal-tension glaucoma), this could influence your risk and the monitoring you should undertake. Each type has its own risk factors and treatment approaches.
c) Yes, recurring eye inflammation (such as uveitis) can increase the risk of developing secondary glaucoma. If you have a history of eye inflammation, it’s important to discuss this with your ophthalmologist.
Final questions
a) A yearly check-up may be sufficient, but if you are at higher risk or show any signs of early glaucoma, you may need to be reviewed by your ophthalmologist more frequently.
b) In SNEC, suitable patients with low risk or stable glaucoma may be reviewed in the Glaucoma Observation Clinic, in which our glaucoma specialists will review their intraocular pressures and glaucoma test results to formulate a management plan, without a physical consultation.
c) Yes, glaucoma can still develop even if eye pressure is normal, especially in cases like normal-tension glaucoma. Regular eye exams are crucial to detect this.
d) Comprehensive testing such as gonioscopy (to examine the drainage angle) or nerve fibre layer analysis (to check the optic nerve health) are typically done as part of the evaluation for glaucoma.
e) Treatment should begin as soon as early signs are detected to prevent vision loss. Early treatment is highly effective at preserving vision.
f) Yes, given your family history, there is a possibility of normal-tension glaucoma. A thorough evaluation and diagnosis by an ophthalmologist are recommended. This form of glaucoma occurs when intraocular pressure is within the normal range, but optic nerve damage still occurs. Regular monitoring is key.
9. Question by Michael
Dear Dr,
When one’s glaucoma has stabilised for a long time, can one be considered to be cured?
Answer by Dr Low Jin Rong
Dear Michael,
Currently glaucoma cannot be cured as the damage to the optic nerve caused by glaucoma is irreversible.
However, it can be managed by slowing down its worsening to prevent further vision loss and to achieve stability of the condition.
10. Question by Kok Too
Dear Low Jin Rong,
I have had visual aura attacks (sometimes with/without headache) since 2024 and occur frequently without warning lasting about 20-30mins each time.
I had seen an eye doctor and no abnormality was observed. My late mother had glaucoma at early eighty. Is it because this visual aura has some risk of getting glaucoma?
Answer by Dr Low Jin Rong
Dear Kok Too,
Visual aura attacks, especially when they occur with or without headaches, are typically associated with migraine aura rather than glaucoma.
Migraine auras are caused by temporary changes in brain activity and blood flow rather than direct damage to the eyes or optic nerve. Migraines, especially with aura, are associated with a slightly higher risk of normal-tension glaucoma.
In addition, since your late mother had glaucoma, you do have a higher genetic risk of developing glaucoma over time.
This risk is independent of your visual aura attacks. Regular eye check-ups will help catch any early signs of glaucoma before vision loss occurs.
11. Question by Donald
Hi Dr Low,
Thank you for taking the time to advise on the managing of glaucoma.
I do use Systane preservative free eye lubricant 2 -3 times a day.
My dad had glaucoma twice, once in his 60s (treated), & another in his late 70s (not yet treated) just before he passed on.
My younger brother (3 years younger) had his in his 40s, hence, I am in my early 60s now & quite concern with this disease as I know it is hereditary.
I have had checks before in 2024 for hazy vision on my right eye, which was diagnosed before as "floaters" years ago.
However, on top of the haziness, on some days, had difficulty to focus with my right eye. Massaging around the right temporal region (nearer to the eye socket) towards the forehead does clear the haziness for a short while.
Sometimes tapping repeatedly on the parietal region with the palms of my hand will work too.
The diagnosis was still the same, due to floaters, & was given "eyelid foam - Naviblef by Novax". Problems did not go away.
Nowadays, the haziness may progress to "frozen vision" if I stare at a subject just after a couple of seconds of longer.
Sometimes, I might experience a slight headache from the top right-side to slightly down backwards on the parietal region. Massaging on these parts brings temporary relief.
I have a scheduled appointment in Apr and am just anticipating that I will be provided with the same prognosis.
What is your initial opinion just based on this information:
a) Do you think it is necessary that more or different test can be done or request during my upcoming visit?
b) Any of these symptoms is/are sign of impending glaucoma?
Answer by Dr Low Jin Rong
Dear Donald,
Thank you for sharing your detailed history. Given your strong family history of glaucoma, ongoing hazy vision, "frozen vision", difficulty focusing and headaches, your concerns are valid. I'll address your questions based on the information provided:
a) Given your symptoms and strong genetic predisposition to glaucoma, a comprehensive eye evaluation may be necessary.
This could include intraocular pressure measurement, gonioscopy, a visual field test, and Optical Coherence Tomography (OCT) of the optic nerve and macula.
It would be beneficial to discuss with your ophthalmologist which investigations are most appropriate in your case.
b) Your symptoms of intermittent hazy vision and headaches may suggest intermittent angle-closure attacks, where partial closure of the drainage angle leads to temporary spikes in intraocular pressure.
If left untreated, this could progress to glaucoma. A detailed evaluation, including gonioscopy, is recommended to confirm or rule out this possibility.
12. Question by Lin Kee
Dear Dr Low,
I am a glaucoma patient. Recently I have developed a bit of floaters on my right eye. Is floater related to my glaucoma? My next check-up is in May 2025. Should I seek doctor's advice before my next appointment? Thank you.
Answer by Dr Low Jin Rong
Dear Lin Kee,
Floaters can be a common occurrence, and they are generally unrelated to glaucoma.
However, if the floaters are accompanied by sudden flashes of light, or if there's a significant change in vision, it's important to seek medical attention as soon as possible.
If the floaters are new and noticeable, a prompt evaluation by an ophthalmologist can help rule out any potential complications, such as retinal tears or detachment, that might require immediate treatment.
13. Question by Ismail
Good day Doctor Low, hope this email finds you well.
I would like to share with you that it has been 3 months that I am experiencing my left eye see object/things differently from my right eye.
My left eye see all object further from my right eye. At the same time, my left eye see colours differently from my right eye. My left eye is seeing a few shades darker than my right eye, e.g. Through my left eye, I am seeing a blue colour as turquoise, while yellow colour is seen as a cream colour.
I have visited an eye doctor for suspected cataract but was told that it was not a cataract. Please help to advise what am I suffering from and is it curable.
Thank you and best regards.
Answer by Dr Low Jin Rong
Dear Ismail,
The symptoms you have described could be due to a variety of conditions, such as a refractive error, early cataracts (not yet detected), retinal conditions, or even neurological issues that affect how the brain processes visual information.
I would suggest a thorough examination of both the retina and optic nerve, and consider further investigations to pinpoint the cause of your visual discrepancies.
14. Question by Mdm Tan
Dear Dr,
I'm 56 years old and have always been prescribed nasal steroid sprays for my sinus related pains. I have family history of glaucoma (mom) so I'm hesitant to use such sprays due to the risk of glaucoma. May I have your views on this please? Thank you.
Answer by Dr Low Jin Rong
Dear Mdm Tan,
Nasal steroid sprays can, in some individuals, lead to an increase in eye pressure over time, which may increase the risk of glaucoma. Given your family history of glaucoma, this is an important consideration.
However, the risk with nasal steroids is generally lower compared to systemic steroids.
I would recommend using the spray cautiously and under the guidance of your ophthalmologist. Additionally, regular monitoring of your eye pressure may be advisable while using the nasal steroids.
15. Question by Janet
Dear Dr. Low and Team, I hope this email finds you well.
My medical history:
I am living with diabetes and hypertension and have been diagnosed with close-angle glaucoma along with a dry eye condition.
I underwent laser treatment for both eyes in 2019, but my intraocular pressure has remained consistently between 19-21 in both eyes.
Occasionally, I experience eye pain and headaches, which can last for half a day or more. Recently, I have noticed increasing blurriness in my left eye.
During my last admission, my eye pressure was recorded as 20 in the left eye and 19 in the right eye, with a mild cataract noted.
My questions are:
a) Is it normal and safe for me to maintain this level of eye pressure? What is my risk of vision loss?
b) Could cataract removal surgery help reduce my eye pressure?
c) How often should I have my eyes checked, and what can I do to reduce my risk?
d) What warning signs should I be particularly concerned about?
I appreciate your time and guidance on these concerns. Looking forward to your advice.
Answer by Dr Low Jin Rong
Dear Janet,
Thank you for sharing your medical history. I hope you are doing well despite the concerns you have raised. I will address your questions point by point below:
a) A normal intraocular (eye) pressure typically ranges from 10-21 mmHg, and your readings are within this range. However, for someone with your history of closed-angle glaucoma, even these levels may still pose a risk, as the eye can sometimes be more sensitive to higher pressure. Ongoing monitoring is critical.
Without careful management, there is a risk of vision loss, though this depends on individual factors, including the degree of optic nerve damage from glaucoma, which can only be assessed through regular check-ups.
b) Cataract surgery can sometimes help lower eye pressure in individuals with closed-angle glaucoma. This is because removing the cataract can open up more space in the eye, allowing better eye fluid drainage and potentially lowering the eye pressure.
However, this effect can vary from person to person, so further evaluation of your case is needed to determine the potential benefit.
c) The frequency of monitoring depends on the severity of your glaucoma and cataracts. Given your current condition and pressure levels, I would recommend having your eyes checked every 3-4 months. However, if your glaucoma progresses or if there are changes in your cataract, we may need to adjust the frequency of monitoring.
To reduce your risk of glaucoma worsening, continue using your prescribed medications, control your blood pressure and blood sugar, and avoid activities that could increase your eye pressure, such as heavy lifting, straining or exercises that involve head-down positions.
d) Please watch for any sudden increases in eye pain, severe headaches, nausea, vomiting, blurred vision, or halos around lights. These could indicate a spike in eye pressure or other complications that need immediate attention. If you notice any of these symptoms, please seek urgent medical care.
16. Question by Anthony
Dear Dr Low, how are you doing?
I have been a glaucoma patient since 2021. I have since operated on both eyes and visited SNEC regularly for reviews. I have also went through a few “needling” on both eyes.
The main issue for both the consultants and patient is the eye pressure. We can measure our own blood pressure at home on a daily basis but not the eye pressure.
Is there a way or a measuring device a patient can use to measure or monitor their own eye pressure at home?
Also, if possible, how can I lower my eye pressure naturally through food (what sort of food) and perhaps our daily activities?
Looking forward to your reply. Thank you.
Answer by Dr Low Jin Rong
Dear Anthony,
At SNEC, we currently have 15 iCare Home Tonometers available for loan to patients. You may consider borrowing one of these devices to measure and monitor your eye pressure at home. Our nurses will provide guidance on how to properly use the device.
Lowering eye pressure through natural methods, such as diet and lifestyle modifications, can complement but not replace medical treatments for glaucoma. Research has identified several foods that may promote eye health, lower eye pressure, or reduce the risk of glaucoma, including green tea, leafy vegetables, citrus fruits (rich in vitamin C), and carrots (high in beta-carotene).
In addition, daily activities that may help lower eye pressure include regular aerobic exercise, proper hydration, sleeping with the head elevated, avoiding excessive caffeine intake, and stress management.
17. Question by Geok
Dear Dr Low,
Good day to you and thank you for taking time to answer our questions.
a) My late father has glaucoma. I was diagnosed with high eye pressure in my early forties and am currently under treatment. My elder sister is in her mid-fifties and her eye pressure is normal. Is there any possibility that glaucoma disease may skip one generation for my sister's case and pass on to her children?
b) My eye pressure hovers around 21 to 24. I went through minimally invasive glaucoma surgery (MIGS) last June for my left eye but unfortunately it did not really help to lower the eye pressure for my case. Does caffeine intake affect the eye pressure? Is it ok to have 2 cups of coffee daily or should I limit to 1 cup or totally remove from my diet?
c) Is it safe for patients with high eye pressure to take the small yellow flu tablet? I was told by the pharmacist at the commercial pharmacy that it may increase the eye pressure and advised that I see a doctor. Is this true?
d) I am using Azarga and recently the doctor added on Xalatan. May I know if I want to use both eye drops together at night, which one should I use first and the interval time between the two?
Thank you very much for your advice.
Answer by Dr Low Jin Rong
Dear Geok,
a) Glaucoma can indeed run in families, and while it is typically more common for it to affect siblings or descendants, it doesn't necessarily affect every generation in the same way.
Glaucoma inheritance is complex and can skip generations, depending on the genetic factors involved. In your sister's case, it’s possible that her eye pressure remains normal, but she could still be at risk of developing glaucoma later in life, especially if there is a strong family history.
It is important for her to have regular eye exams, as early detection is key to managing glaucoma. If she has children, they may inherit a higher risk and should also be monitored closely as they age.
b) Caffeine can have a temporary effect on eye pressure. Some studies suggest that caffeine may cause a short-term increase in eye pressure, especially in individuals who already have elevated eye pressures.However, the effect is usually modest and temporary, and regular moderate caffeine consumption is generally considered safe for most individuals with glaucoma.
In your case, where your eye pressure ranges between 21 to 24 mmHg, having one or two cups of coffee daily may not significantly affect your long-term management, but it might be worth trying with a reduction (e.g., limiting to one cup) to see if it helps to stabilise your eye pressure.
You could also consult your eye doctor to see if they recommend reducing caffeine intake based on your specific case and treatment plan.
c) The small yellow flu tablet which you mentioned may typically contain pseudoephedrine or similar decongestants, which can increase eye pressure, especially in individuals with glaucoma or elevated eye pressures. Pseudoephedrine, a common ingredient in cold and flu medications, can cause pupil dilation and reduce fluid drainage from the eye, potentially increasing eye pressure.
It is important to check the active ingredients in any flu medication and consult your doctor or pharmacist before taking them. Your pharmacist’s advice to consult with a doctor is valid, as some flu medications can indeed raise eye pressure and may not be safe for individuals with glaucoma.
d) When using two different eye drops like Azarga and Xalatan, it's important to space them out to avoid any potential interaction between the two medications and to ensure maximum effectiveness.
Here is the general guideline for using both:
Xalatan should typically be used first. This is because it is a prostaglandin analogue, and it is usually recommended to be applied before other eye drops to ensure it works effectively without being diluted by the other medications.
Azarga can then be used after a 5-10 minute interval. This waiting time helps prevent the drops from mixing and ensures that each medication has enough time to absorb into the eye.
So the recommended order is:
First, apply Xalatan.
Wait for 5-10 minutes.
Then, apply Azarga.
It is always a good idea to confirm this with your eye doctor or pharmacist as well, especially if there are any specific recommendations for your situation.
Ref: G25
Related article:
Glaucoma: The Silent Thief of Sight
