Macular degeneration is a age-related condition of the retina. The Vitreo-Retinal Department at Singapore National Eye Centre (SNEC) discusses some important facts.
Age-related Macular Degeneration (AMD) is one of the leading causes of blindness affecting those 50 years or older.
Macular degeneration or
Age-related Macular Degeneration (AMD for short) is a chronic eye condition that often results in vision loss in the centre of the visual field because of damage to the macula (the central part of the retina). Some of this vision loss may be permanent or irreversible.
This condition may make it difficult for the patient to read, recognise faces or drive safely, because we rely on our central vision for these tasks.
However, as AMD hardly affects peripheral vision, those that suffer from it are usually able to remain independent to perform most daily activities.
2 types of Age-related Macular Degeneration (AMD)
Age-related Macular Degeneration (AMD) occurs in "dry" and "wet" forms.
90% of AMD patients suffer from the "dry" form. Patients with dry AMD may have no symptoms, or may experience slow progressive loss of central vision. Vision is affected as the light-sensitive cells in the macula slowly break down with age.
Wet AMD, also known as exudative or neovascular AMD, is caused by the growth of small, abnormal blood vessels under the retina in the macula. Wet AMD usually arises from pre-existing dry AMD. These abnormal blood vessels leak blood, fluid, lipids and protein, resulting in disruption of the normal structure of the retina.
If it is not treated, scar tissue tends to form under the macula, resulting in permanent central vision loss. The "wet" form of AMD is more aggressive, and often results in severe visual loss within a short period of time.
Age-related Macular Degeneration (AMD): Is it preventable?
So far, there are no treatments that have been proven to be highly effective in preventing Age related Macular Degeneration (AMD).
A particular combination of supplements and vitamins, commonly referred to as the "AREDS2" formulation, has been shown to reduce the risk of developing the advanced form of AMD. However, the reduction in risk was only about 25% over 5 years, and this was only proven for some patients with high risk, and not all patients. It would be best to consult your eye doctor on whether these supplements will be beneficial for you.
The best way to avoid permanent vision loss is with prompt eye examination and diagnosis by your eye doctor. Early diagnosis improves the chances of treatment success.
"In its early stages, tiny yellow spots known as drusen may appear underneath a patient’s retina, which can be detected by an opthalmologist with an eye examination.
Although the drusen are early signs of AMD, most cases the patients retain good vision and only a small number progress over many years to the serious sight threatening forms of AMD," said Clinical Associate Professor Anna Tan, Senior Consultant, Medical Retina Department, Singapore National Eye Centre (SNEC), a member of the SingHealth group.
Did you know? Studies have shown that
smokers are more than four times at greater risk of developing "wet" or advanced Age-related Macular Degeneration (AMD) than non-smokers. Therefore, reducing or stopping smoking can reduce the risk of AMD.
|
Symptoms of Age-related Macular Degeneration (AMD)
In early Age-related Macular Degeneration (AMD), the impact on vision is generally mild or even non-existent. However, as the disease progresses, symptoms may include:
Blurring of central vision (may be gradual or rapid in onset)
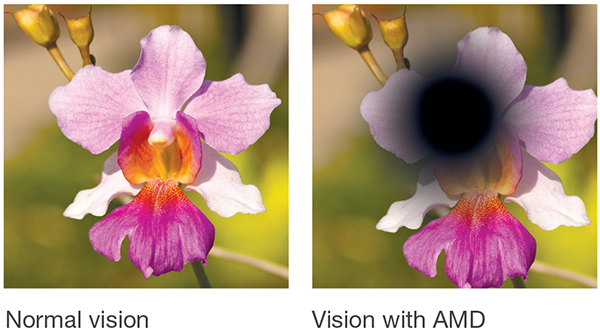
Shadows or missing areas of vision
Distorted vision (e.g. straight lines appear wavy)
Problems discerning colours, especially differentiating between similar colours
Slow recovery of visual function after exposure to bright light
Loss of contrast sensitivity (ability to tell different levels of brightness apart)
Risk factors for Age-related Macular Degeneration (AMD)
A person's risk of getting AMD increases with:
Age-related Macular Degeneration (AMD): How to diagnose
The early stages of AMD usually start without
symptoms. Only a comprehensive dilated
eye examination can detect AMD. The eye
examination may include the following:
1) Amsler grid
Your ophthalmologist may ask you to look
at an Amsler grid. Changes in your central
vision may cause the lines in the grid to
disappear or appear wavy, a sign of AMD.
This is also used to monitor patients at
home for progression.
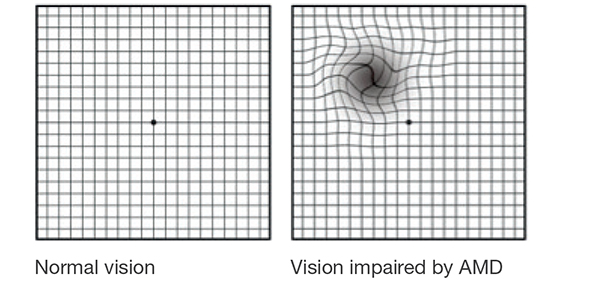
How is the test performed: Hold the Amsler grid below at eye level at a comfortable
reading distance. If you wear any type of reading lenses,
wear them during this test. Cover one eye at a time, and
focus on the centre dot. If you see wavy or fuzzy lines,
or if certain squares are missing or appear blurred, you
may be displaying symptoms of AMD.
2) Fundus Fluorescein Angiogram
(FFA) and Indocyanine Green
Angiogram (ICG)
In this test, a fluorescent dye is injected
into a vein in your arm. Pictures are taken
as the dye passes through the blood vessels
in your eye. This makes it possible to see
leaking blood vessels, which occur in the “wet”
type of AMD.
In rare cases, complications
due to the injection can arise, like nausea or
more severe allergic reactions
3) Optical Coherence Tomography (OCT)
You have probably heard of ultrasound,
which uses sound waves to capture
images of living tissues.
OCT is similar
except that it uses light waves, and can
achieve very high-resolution cross-
sectional images of any tissues that can
be penetrated by light, such as the eyes.
After your eyes are dilated, you will be
asked to place your head on a chin rest
and hold still for several seconds while
the images are obtained. The light beam
is painless.
Click on page 2 to read about
how macular degeneration is treated.
Ref. G25 (ed)
Check out other articles on eye care:
Our Eyes - Our Window to the World
Childhood Myopia and How Atropine Eye Drops Can Help
Common Strabismus in Children
LASIK: Is It Suitable For You?
Cataract: Causes, Symptoms and Treatment
AMD (Age-Related Macular Degeneration): What You Need to Know
Glaucoma: The Silent Thief of Sight
Eye (Ocular) Inflammation: What Causes It?
What Causes Optic Neuritis (Optic Nerve Inflammation)?
What is Diabetic Retinopathy?
Aesthetic Eye Surgery: Everything You Need to Know
