Being unable to play your favourite sport can be a big blow if your life revolves around it. When his doctor stopped him from playing competitive rugby after he sustained multiple injuries and tore two neck ligaments in 2011, Mr Toh Kiat Sheng gradually lost the discipline to exercise.
His physical health began to deteriorate and his weight increased from 80 kg to 120 kg as he started binge-eating for comfort. A 5-minute walk made him breathless, which further affected his self-esteem.
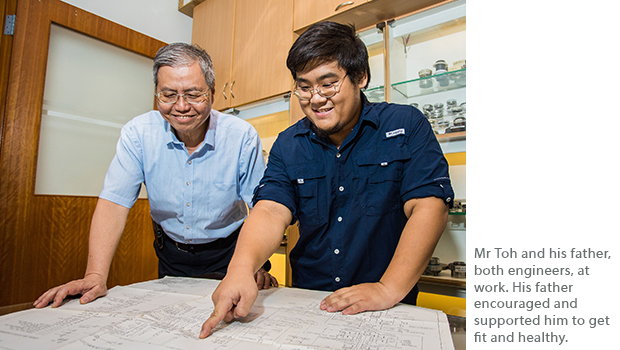
When his father alerted him that the skin around his neck was starting to turn dark - a possible sign of diabetes, Mr Toh went to Tampines Polyclinic for consultation and advice. The Polyclinic referred him to the Weight Management Programme at the SingHealth Duke-NUS Sport & Exercise Medicine Centre (SDSC) at Changi General Hospital (CGH). He roped in his older brother, Mr Toh Kiat Boon, and together the two siblings started on the programme.
Personalised care from a multidisciplinary team

Both brothers found the multidisciplinary care highly effective in helping them develop a holistic weight management plan tailored to their lifestyles. The younger Mr Toh was introduced to a team comprising Dr Leonard Lim Ang Tee, a Sport and Exercise Medicine Consultant at CGH, Ms Miko Yeo, a dietitian, and Mr Zack Teng, an exercise physiologist.

The team worked hand-in-hand to ensure that the advice they gave Mr Toh was relevant to his specific healthcare needs. “We work closely as a team and have regular update sessions on each patient’s progress to see how we can help them achieve their goals,” said Dr Lim.
One example of the healthcare team personalizing the care plan to suit Mr Toh’s lifestyle was when dietitian Ms Yeo asked him to keep a food diary for a few days before working with him to come up with a customised diet plan. Ms Yeo said, “Looking at his food diary, I saw that he enjoys meat and rice dishes so I suggested healthier alternatives like stir fried meat dishes, with half a bowl of brown rice. That way, he still gets to enjoy what he likes, but with a lower calorie intake.“

Similarly, exercise physiologist Mr Teng formulated an exercise regime that Mr Toh was able to do and was comfortable following. “We used Mr Toh’s knowledge of physical training from his rugby days to come up with a suitable exercise regime. This allowed him to better identify with the exercises, thereby facilitating better continuity and adherence,“ explained Mr Teng. Along with the diet and exercise plans, Dr Lim regularly assessed Mr Toh’s medical condition and kept a close eye on his progress to make sure he was exercising safely and effectively.

The nine SingHealth Duke-NUS Disease Centres (SDDCs) are models of care that leverage the resources of the cluster for patients with specific conditions who require multidisciplinary care. Adj Assoc Prof Benedict Tan, Head of the SDSC and Chief of the Sport and Exercise Medicine Department at CGH, said, “CGH is not the only SingHealth facility that offers comprehensive weight management programmes. SGH Life Centre, KKH and others have such capabilities as well. If the overweight patient is in his teens, then he would be referred to KKH. If the overweight patient has poorly controlled diabetes, he would be referred to an endocrinology-led programme like the one at SGH Life Centre,” explained Adj Assoc Prof Tan.
Empowering patients to take charge of their health

Weight management requires a lifelong commitment to lifestyle changes and patient involvement is critical. As education is key to empowering patients to make the right choices, the SDSC team focuses on equipping patients with resources and tools to lead a healthier lifestyle, after their discharge from the 6-month weight management programme.
For example, Ms Yeo makes it a point to teach patients how to read food labels and select food products with essential nutrients. She also shares useful websites which have reliable educational materials.
“Before the programme, I relied on what I found on the internet and didn’t really know where to get accurate information. At first, I wanted to go on a no-carbohydrate diet but thankfully, the dietitian suggested a safer alternative and gave me information to help me do it. The best part is having healthcare professionals who help and empower me to make the right decisions. These are tools I can use for the rest of my life.” Mr Toh said.

Along with a caring father who accompanies him for evening walks and gets rid of unhealthy snacks around the house, feeling fitter and healthier has served as Mr Toh’s motivation. He has lost more than 30 kg since enrolling on the weight management programme and now takes a daily walk to and from work every day without feeling breathless.
Having been deeply involved in his own care journey, Mr Toh knows the importance of being empowered and supported to keep well and stay healthy. Yet, he admits it can be an uphill struggle to embark on the journey to health.
“You just have to dig deep and find the discipline to get healthy and stay well,” Mr Toh advised.
SINGHEALTH DUKE-NUS DISEASE CENTRES
What are SDDCs?
SingHealth Duke-NUS Disease Centres (SDDCs) are strategic models of care for patients with specific conditions who require multidisciplinary teamwork. The structure enables professionals from different disciplines and institutions to work closely together to enhance care. SDDCs provide quality clinical care throughout the care continuum and improve outcomes. In conventional care, a patient with a nodule (growth of abnormal tissue) in his neck may be referred to a thyroid specialist or surgeon, who would then refer him to a diagnostic radiologist for imaging tests. If the nodule is found to be a cyst, the patient would be given an appointment for a biopsy. By this time, the patient would have made multiple trips to the hospital to see different specialists. With the SDDCs, the patient’s journey is streamlined, cutting down the number of visits, and saving time and money. It also translates to greater efficiency for the care team.
For Tomorrow’s Medicine
The SDDCs’ approach to collaborative care places emphasis on developing a comprehensive database for care and research. In the long term this will change the way treatment is recommended as outcomes are collectively measured and studied to continuously improve protocols.
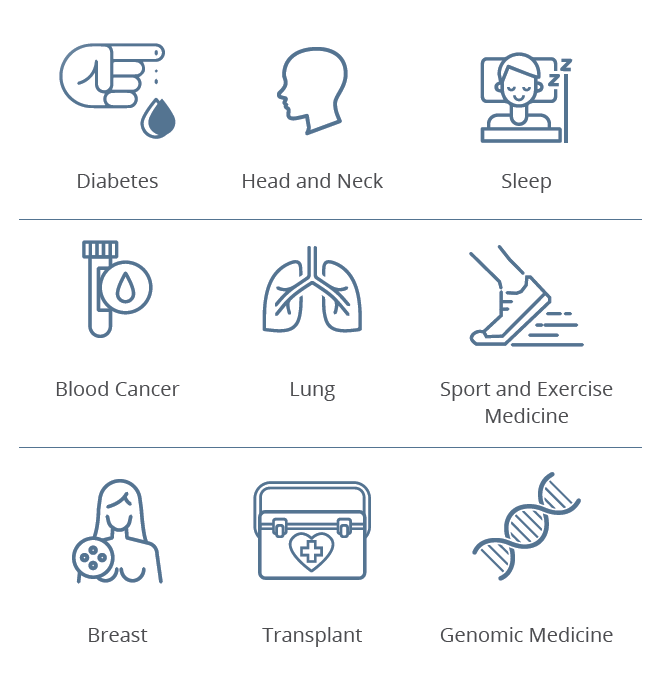
Our SDDCs
9 SDDCs that leverage multidisciplinary coordination to enhance care have been established.
FY2018 Highlights
Head & Neck Centre
Enhanced programmes and services were implemented upon the return of the Head & Neck Allied Health Professionals (AHP) faculty team from HMDP Fellowship. Some examples include the introduction of a cancer survivorship programme, increased capacity with more services offered at the combined multidisciplinary clinics and improved wound management and early rehabilitation protocols for surgery preparation and recovery. These initiatives have helped to improve the quality of care for patients. New research infrastructure has also been set up to track surgical outcomes and facilitate greater collaboration between head and neck surgeons, nurses and allied health professionals.
Lung Centre
The Lung Cancer Consortium from NCCS secured a $10-million collaborative grant at the National Medical Research Council (NMRC) Awards 2018, boosting research efforts. Two clinician scientists from the Lung Centre also clinched awards at the NMRC Awards 2018 for their outstanding contributions. The SGH Lung Endoscopy Centre and the SGH-SKH Chronic Obstructive Pulmonary Disease Clinic were the first team in Southeast Asia and the second in Asia to perform bronchoscopic segmental lung volume reduction for patients with advanced emphysema. They have since trained interventional pulmonologists from the region.
Breast Centre
With all the Breast Units across SingHealth completing the move to the Breast Centre in 2018, a centralized SingHealth Breast Cancer Registry is currently being developed to measure outcomes, aid research and advance value care. The Breast Care Nurse Specialty Course will have its first intake in FY2020 to train nurses to advance their skills in breast cancer care through e-learning and clinical attachment.
Diabetes Centre
In September 2018, the Diabetes & Metabolism Centre Dental Clinic was established to provide preventive dental care for patients with diabetes as they are at higher risk of developing periodontal disorders.
Blood Cancer Centre
A pilot project was implemented in August 2018 at NCCS and SGH lymphoma clinics to assess cost effectiveness of patient care for Diffuse Large B-cell Lymphoma patients. In October 2018, a multidisciplinary fellowship team comprising staff from SGH and KKH travelled to Toronto under the Health Manpower Development Plan to learn about survivorship and long-term follow-up programmes for young people with malignant and benign haematological conditions, who are transiting to the adult haematology programme.
Sleep Centre
The Sleep Centre officially launched the Sleep Clindoc, an electronic data input system, in March 2019 to harmonise patient care, clinical data input and collection, allowing clinicians to conduct research with the SingHealth Duke-NUS Sleep Registry in the near future. The Centre successfully attained the Ministry of Health’s (MOH) approval for the subsidy of Home Sleep Study to diagnose patients with obstructive sleep apnea, nation-wide. This will help reduce the waiting time for diagnosis and treatment of obstructive sleep apnea. The SingHealth Duke-NUS Sleep Centre-Philips Sleep Medicine Course was established to train healthcare professionals from Asia Pacific in sleep medicine.
Sport and Exercise Medicine Centre
In line with MOH’s nationwide war on diabetes, CGH launched the Health Peers Programme, in partnership with community stakeholders and government agencies and received the PA Community Partnership Excellence Award 2018 in recognition of its efforts. CGH Sport and Exercise Medicine and NTU Lee Kong Chian School of Medicine developed and launched the Graduate Diploma in Sports Medicine programme for doctors – the first and only in Singapore and Asia.
Transplant Centre
The Transplant Centre was launched in April 2019 to amalgamate all transplant programmes in SingHealth. The centre aims to double transplant survival, optimise the quality of patients’ lives and improve access and affordability. The Liver Transplant Centre is now part of the new Transplant Centre.
Genomic Medicine Centre
The Genomic Medicine Centre was newly formed in 2019 to benefit patients with genetic diseases. The Centre aims to be a global leader in delivering state-of-the-art clinical care by using advanced genomic technologies to improve patient diagnostics, therapeutics and healthcare outcomes. |