
Tubal ligation, a contraceptive procedure where a woman’s fallopian tubes are surgically blocked or severed, is one of the most prevailing contraceptive options due to its high success rate (more than 99%). Women who desire more children after undergoing tubal ligation can consider two options to achieve pregnancy: in-vitro fertilisation (IVF), or microsurgical reversal of ligation – which is also known as tubal reversal.
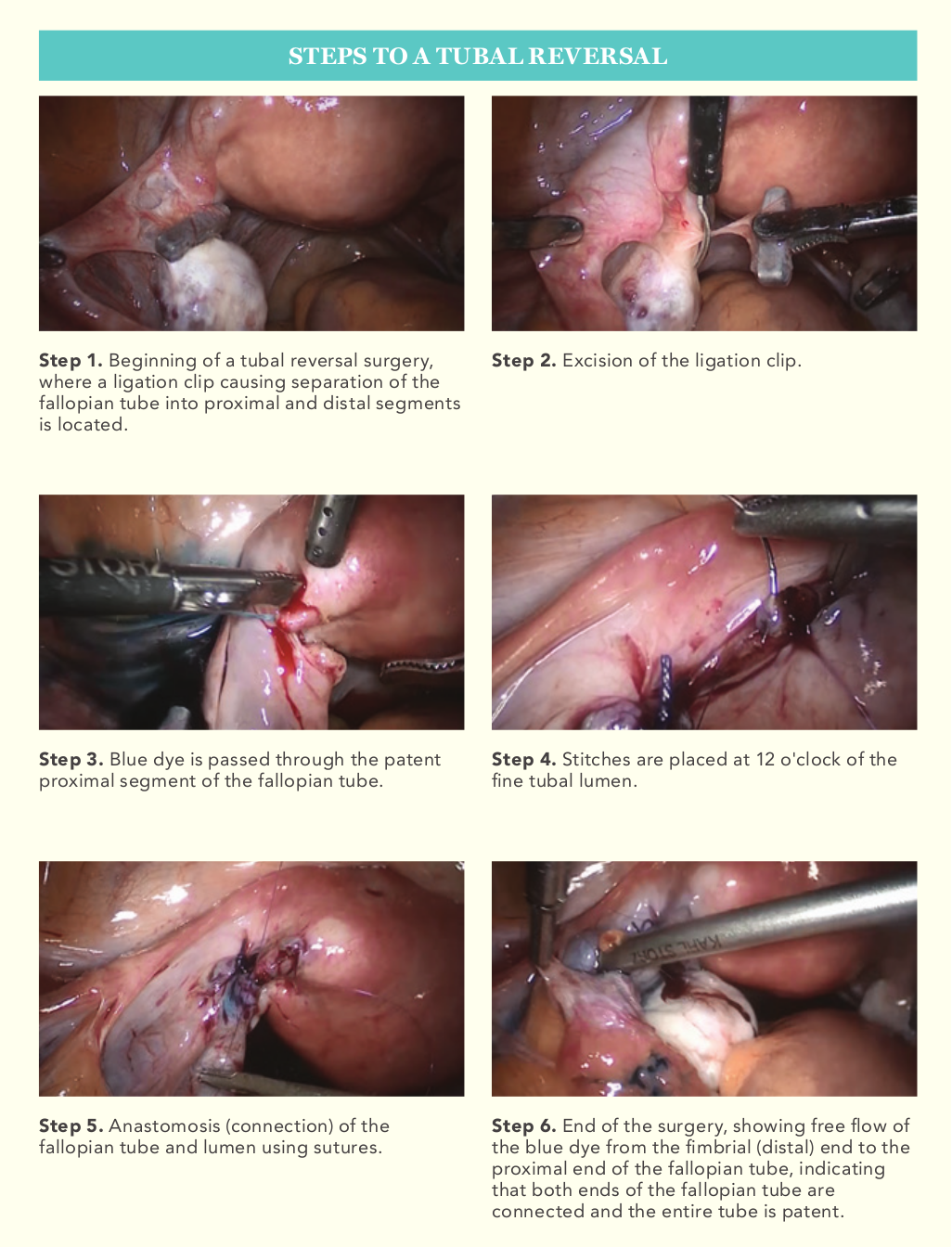
Tubal reversal is a delicate microsurgical procedure involving the excision of the scarred segment of a fallopian tube and the precise anastomosis (connection) of the healthy proximal and distal ends of the tube. As the fallopian tube has a very fine lumen, precise anastomosis is crucial for a successful outcome. Hence, medical professionals would require intensive training to acquire proficiency in this delicate procedure. The procedure can be done under laparoscopy, allowing rapid recovery and discharge from the hospital.
Restoring natural fertility through tubal reversal
In recent times, with improvements to IVF techniques and pregnancy outcomes, the role of tubal reversal in enabling pregnancy after ligation has come under scrutiny, with many patients and physicians preferring the IVF route.
However, KK Women’s and Children’s Hospital (KKH) has observed good results in patients who have undergone tubal reversal. The KKIVF Centre has seen up to 70 to 80 per cent chance of pregnancy in properly screened patients after undergoing tubal reversal through laparoscopy. As with all surgeries, tubal reversal is not without its risks, namely surgical risks and a higher risk of subsequent ectopic pregnancy.
Nonetheless, the main advantage of tubal reversal is that it allows women to have sustained chance of pregnancy with every menstrual cycle, compared to limited attempts with IVF.
Studies comparing these two methods have also shown tubal reversal to be significantly more effective in women less than 40 years of age1. Hence tubal reversal is ideal for younger women with a reasonable chance of cumulative live births.
To optimise the chances of achieving pregnancy post-procedure, a couple requesting tubal reversal should have good natural fertility – preferably below the age of 40 years and with a healthy body mass index – the woman should have a good ovarian reserve, and the man should have a normal sperm count.
Case study: A second chance at pregnancy through tubal reversal
Thirty-one-year-old Amy (not her real name) had undergone surgical sterilisation by ligation of her fallopian tubes after delivering her second child.
At the reproductive medicine clinic at KKH, Amy was presented with two choices to manage her subfertility – in-vitro fertilisation (IVF) or reversal of tubal ligation. She initially opted for IVF and underwent one IVF cycle, which turned out to be unsuccessful. Ten years later, she decided to try for a third child.
Subsequently, Amy decided to undergo a laparoscopic reversal of tubal ligation. During the operation, she was found to have signs of pelvic inflammatory disease: adhesions at the liver (Fitz-Hugh-Curtis syndrome) and around the tubes and ovaries. This caused further scarring and shortening of the fallopian tubes, on top of damage from the previous ligation. Despite this, the KKH surgeon was able to successfully reconstruct Amy’s fallopian tubes.
Two months after the surgery, an ultrasound scan confirmed a healthy pregnancy. Amy is currently receiving antenatal care in KKH.
In this classic case study, IVF would have been instinctively the preferred choice for many, given the fact that pelvic inflammatory disease was present. In theory, the patient’s fallopian tubes would have been damaged and unable to transport sperm and eggs effectively.
However, through laparoscopic reversal of tubal ligation, the medical team was able to treat the patient’s pelvic inflammatory disease by excising adhesions and unhealthy portions of her fallopian tubes – successfully restoring the function of her fallopian tubes and enabling a pregnancy.
Refer a patient
Polyclinics and community healthcare practitioners can contact KKH at
+65 6294 4050 to refer patients to the Reproductive Medicine Clinic for consultation and tertiary evaluation on their eligibility for tubal reversal. |

|
Dr Chua Ka-Hee, Associate Consultant, Division of Obstetrics and Gynaecology, KK Women’s and Children’s Hospital Dr Chua Ka-Hee works closely with the Department of Reproductive Medicine at KKH, and has a special interest in male subfertility. Dr Chua is also a member of the Royal College of Obstetricians and Gynaecologists. |

|
Associate Professor Tan Heng Hao, Head and Senior Consultant, Department of Reproductive Medicine, KK Women’s and Children’s Hospital Associate Professor Tan Heng Hao is Head of the Department of Reproductive Medicine, and Deputy Chairman of the Division of Obstetrics and Gynaecology at KKH. He is also the Director of the KKIVF Centre and the National Sperm Bank. Passionate about education, A/Prof Tan is the Section Chair of Reproductive Medicine in the College of Obstetricians and Gynaecologists, Singapore, and was awarded the KK People Developer Award for Outstanding Clinical Teacher in 2013. |
Reference: - Tan HH, Loh SF. Microsurgical reversal of sterilisation - is this still clinically relevant today? Ann Acad Med Singapore. 2010 Jan; 39(1):22-6.
|

