When GPs are presented with thyrotoxicosis, radioactive iodine can be a useful adjunct for imaging to aid in its diagnostic management, as well as for treatment. Singapore General Hospital shares more.
When general practitioners are presented with thyrotoxicosis in their practice, radioactive iodine can be a useful adjunct for imaging to aid in its diagnostic management, as well as for treatment. Singapore General Hospital shares more about the indications for referral and shared care with GPs post-treatment.
INTRODUCTION TO THYROTOXICOSIS
Thyroid diseases encompass a wide variety of
problems seen at the primary healthcare setting,
and experts estimate that up to 5 to 10 percent of the
population suffer from a thyroid disorder. In particular,
patients with thyrotoxicosis are commonly presented
to the general practitioner (GP).
Causes of thyrotoxicosis
The causes of thyrotoxicosis may include:
- Graves’ disease
- Toxic adenomas
- Toxic multinodular goitre (+/- compressive
symptoms)
- Thyroiditis
- Factitious hyperthyroidism
The goals of managing thyrotoxicosis would be to
determine the aetiology as appropriate management depends on the underlying mechanism.
The most common cause of endogenous thyrotoxicosis
(hyperthyroidism) would be Graves’ disease, also
known as diffuse toxic goitre. Graves’ disease is an
autoimmune condition affecting the thyroid that usually
occurs in young to mid-adulthood, and in women more
than men.
Up to 30% of patients with Graves’ disease suffer from
Graves’ ophthalmopathy, and smokers are more prone
to thyroid eye disease.
WHAT IS RADIOACTIVE IODINE (RAI)?
Iodine is a chemical element, and this trace mineral is
found naturally in the environment and many foods.
Its clinical significance lies in the fact that the body
uses iodine to make thyroid hormones which control
metabolism.
There are many radioisotopes of iodine, of which I-123
and I-131 are important for imaging and therapeutics respectively.
RAI IMAGING OF THE THYROID
How it works
Thyroid imaging and treatment capitalise on the
process of hormone synthesis in the glands. This is
dependent on the sodium-iodide symporter (NIS). Via
the NIS, RAI gets trapped intracellularly. Radioiodine is
then organified to form thyroid hormones (T3 and T4).
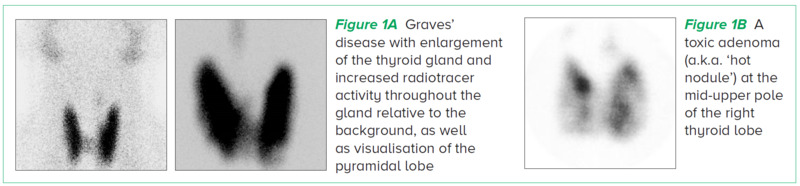
The images in Figure 1 show common causes of
hyperthyroidism and their appearances.
Its role in thyrotoxicosis management
The role of thyroid nuclear imaging referred from
the primary care setting will mainly be to relate the
general structure of the gland to function. This will
be particularly useful in differentiating the causes
of thyrotoxicosis such as Graves’ disease from toxic
nodular goitre or thyroiditis.
In Singapore, almost all healthcare institutions
will usually use a different radiotracer, Tc-99m
pertechnetate, as an imaging substitute for RAI thyroid
scintigraphy as it is more easily accessible and has a
shorter radiation half-life.
At Singapore General Hospital (SGH), our team will
routinely pair thyroid nuclear imaging with a correlative
ultrasound as an adjunct, and also for anatomical
correlation.
WHO SHOULD BE REFERRED FOR RAI
THERAPY OF THE THYROID
Indications for RAI therapy of hyperthyroidism
due to Graves’ disease, toxic multinodular goitre or
adenoma
- Refractory to medical therapy
- Relapsed cases previously on medical therapy
- Allergy to antithyroid drugs
- Unsuitable for surgery
RAI is the most commonly used hyperthyroid treatment
in the United States.
Contraindications to using RAI for therapy
-
Hypersensitivity reaction to iodine
- Pregnancy or planning a pregnancy within
4 to 6 months
- Breastfeeding (patient will have to give up
breastfeeding for that infant if RAI is given)
- Uncontrolled hyperthyroidism with FT4 > 30
(relative contraindication – will need better
control before elective RAI therapy)
- Severe Graves’ ophthalmopathy
Do consider providing opportunistic smoking cessation
advice to any patients referred for RAI therapy.
POSSIBLE SIDE EFFECTS AND
COMPLICATIONS OF RAI THERAPY
- Nausea
- Metallic taste in mouth
- Salivary gland swelling and discomfort
- Transient discomfort of thyroid gland
+/- rise in thyroid hormone levels
- Thyroid storm (rare)
- Aggravation of pre-existing Graves’
ophthalmopathy (rare)
On occasion, we may refer some patients for an
ophthalmology assessment prior to RAI therapy
should it be required.
Patients have to be counselled that they may
develop hypothyroidism after RAI thyroid ablation
necessitating lifelong thyroxine replacement, but this
is the intended aim rather than a side effect.
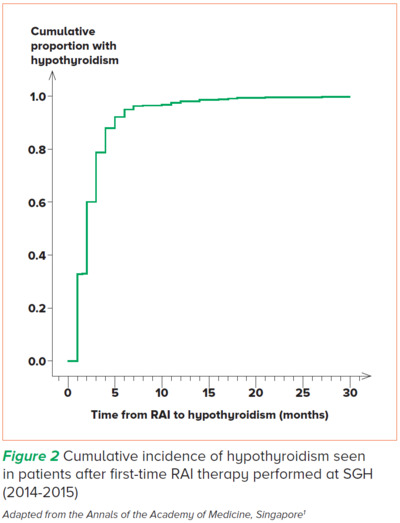
EFFICACY OF RAI THERAPY
Treatment with RAI is efficacious and the majority of
individuals have a successful clinical outcome, with
most patients rendered hypothyroid within a few
months after first-time RAI therapy.
A larger goiter size and thyroid stimulating hormone
receptor antibody (TRAb) positivity at RAI may predict
failure of first-time RAI therapy necessitating a second
treatment.
Patients are discharged back to their primary care
provider once they are hypothyroid and started on
thyroxine replacement.
PREPARING FOR RAI THERAPY IN SGH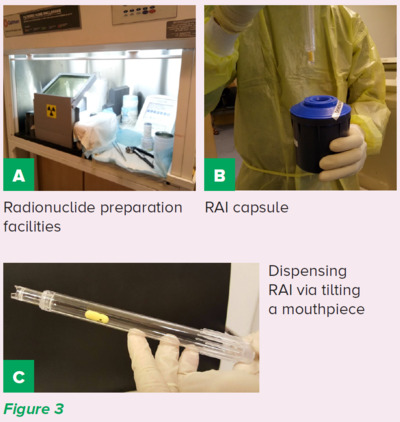
Patient preparation
After clinical consultation, our team of doctors and
nurses will provide comprehensive counselling for
RAI dose preparation with regard to medications
and low iodine dietary advice.
Patients will be provided with a detailed pamphlet
to help allay patient concerns regarding
radiation exposure. They will also be given a
set of instructions for what to do and what to
avoid regarding radiation exposure to family
and members of the public post-treatment as an
outpatient.
No hospitalisation is needed with the low levels of
RAI activity prescribed for hyperthyroidism.
RAI preparation
The RAI capsule or liquid is ordered by the
laboratory and will require a three-week lead time
(usually sourced from Europe). Upon its arrival,
over the weekend, the relevant quality control
and dose activity checks will be performed. It will then be placed securely in a lead-shielded area
ready for outpatient administration on a weekday
afternoon (Figure 3).
CONCLUSION
RAI is a useful adjunct for imaging to aid in the
diagnostic management of patients presenting to
the GP with thyrotoxicosis. In addition, RAI is one of
the mainstays of treatment for hyperthyroidism with
the preferred clinical outcome of lifelong thyroxine
replacement rather than prolonged treatment with
anti-thyroidal drugs.
After successful treatment with RAI, patients will be
discharged back to their primary healthcare provider
for further titration of thyroxine and long-term follow-up.
GPs can call the SGH Department of Nuclear
Medicine and Molecular Imaging for appointments
at 6321 4203 or 6321 3838.
REFERENCE
-
Tay WL, Chng CL, Tien CS, Loke KS, Lam WW, Fook-Chong SM, Tong AK. High Thyroid Stimulating Receptor Antibody Titre and Large Goitre Size at
First-Time Radioactive Iodine Treatment are Associated with Treatment Failure in Graves’ Disease. Ann Acad Med Singap. 2019 Jun;48(6):181-187.
Dr Aaron Tong is a Senior Consultant and Director of Nuclear Medicine Operations at the
Department of Nuclear Medicine and Molecular Imaging, Singapore General Hospital. He
is also a Visiting Consultant and Clinical Governance Officer (Nuclear Medicine) at the
Department of Radiology, Sengkang General Hospital.
He received his specialist accreditation in nuclear medicine in 2015 and serves as the
current Chairman in the Chapter of Nuclear Medicine Physicians, Academy of Medicine
Singapore. He has a keen interest and takes an active role in various research and educational activities.
Dr Tham Wei Ying is a Consultant Nuclear Medicine Physician at Singapore General
Hospital. She completed her nuclear medicine senior residency at SingHealth in 2018 and has been with the Department of Nuclear Medicine and Molecular Imaging since. She
maintains a broad interest in both diagnostic and therapeutic nuclear medicine scans and procedures. She is also actively involved in education and is a core faculty member of the
nuclear medicine senior residency programme.
GP Appointment Hotline: 6326 6060
GPs can find out more information about the department here.
