General practitioners are key to identifying potential thyroid malignancies. The SingHealth Duke-NUS Head & Neck Centre shares more about the latest in assessment and treatment options, and when specialist referral is needed.
Thyroid nodules are usually incidentally picked up during health screenings in the primary care setting. General practitioners are therefore key to initiating investigations to identify potential malignancies. Find out more about the latest in assessment and treatment options, and when specialist referral is needed.
INTRODUCTION TO THYROID NODULES
The occurrence of thyroid nodules is very common, and
it has been shown that nodules can be detected with
ultrasound (US) in up to 68% of a random population,
with increased incidence in females and the elderly1.
Most of these patients with thyroid nodules are
asymptomatic, with the nodules being picked up
incidentally on routine head and neck imaging for
other conditions, or via US done during health
screening in the primary care setting.
Incidence of thyroid cancer
Fortunately, the vast majority of thyroid nodules
(> 95%) are benign and do not cause problems in
the patients’ lifetimes. Congruent with the increased
detection of thyroid nodules, the incidence of thyroid
cancer is also increasing globally.
In Singapore, thyroid cancer is the eighth most
common cancer amongst females, with an incidence
of 10.9 per 100,000 individuals. Of note, amongst
younger females less than 50 years of age, it ranks in the top three commonest malignancies.
The priorities in the evaluation of patients with
thyroid nodules will therefore be to exclude
malignancy and to identify symptomatic patients
who may benefit from intervention.
CLINICAL PRESENTATION
Figure 1 shows the symptoms, signs and red flags to look out for in the presentation of thyroid nodules.
| Symptoms and signs | Red flags |
Anterior neck swelling:
Dominant nodule, goitre Compressive symptoms:
Dysphagia, dyspnoea
(typically worse when lying down) Hormonal dysfunction:
Symptoms/signs of thyrotoxicosis or hypothyroidism Assess for risk factors:
Previous neck irradiation, family history
of thyroid malignancy
| Voice hoarseness Rapidly enlarging swelling Presence of lymphadenopathy Significant compressive symptoms –
airway distress Fixation of nodule to surrounding tissues
|
Figure 1
TYPES OF INVESTIGATIONS
1. Thyroid function test
When it is needed
A thyroid function test (TFT) should be performed
in the initial assessment of a patient with a thyroid
nodule or goitre, especially if they have symptoms
suggestive of thyroid hormonal dysfunction.
Managing thyroid hormonal dysfunctions
The treatment of hyperthyroidism or hypothyroidism
can be initiated in the primary care
setting and these patients can continue to follow
up with their general practitioners once their
thyroid function is controlled.
For patients with thyroid functions that are more
difficult to control, or in the presence of red flags or
atypical features, referral for specialist evaluation
should be considered.
2. Thyroid ultrasound
When it is needed
A US of the thyroid with evaluation of lymph nodes
should be performed in all patients presenting with
thyroid nodules or goitres.
Objectives
The objectives of ultrasonography are to:
- Confirm the clinical diagnosis
- Evaluate the size of the nodules/goitre
objectively (allowing a baseline for
surveillance)
- Assess for suspicious features that will
necessitate further investigation with a fine
needle aspiration cytology
Standardised scoring system
However, US reports, until recently, lacked standardisation
and can be difficult to interpret. Tracking nodules across various time points can also be
challenging.
Since mid-2022, the reporting of US thyroids
in SingHealth has followed a similar format
regardless of performing institution. Nodules are
labelled the same way on follow-up scans.
In addition, nodules are now reported according
to the Thyroid Imaging Reporting & Data System
(TI-RADS)2 (Figure 2) . TI-RADS is a scoring system
which has been validated for reproducibility with
clear criteria for nodule sampling, allowing a more
streamlined approach. There is also evidence to
show that it has reduced sampling rates.
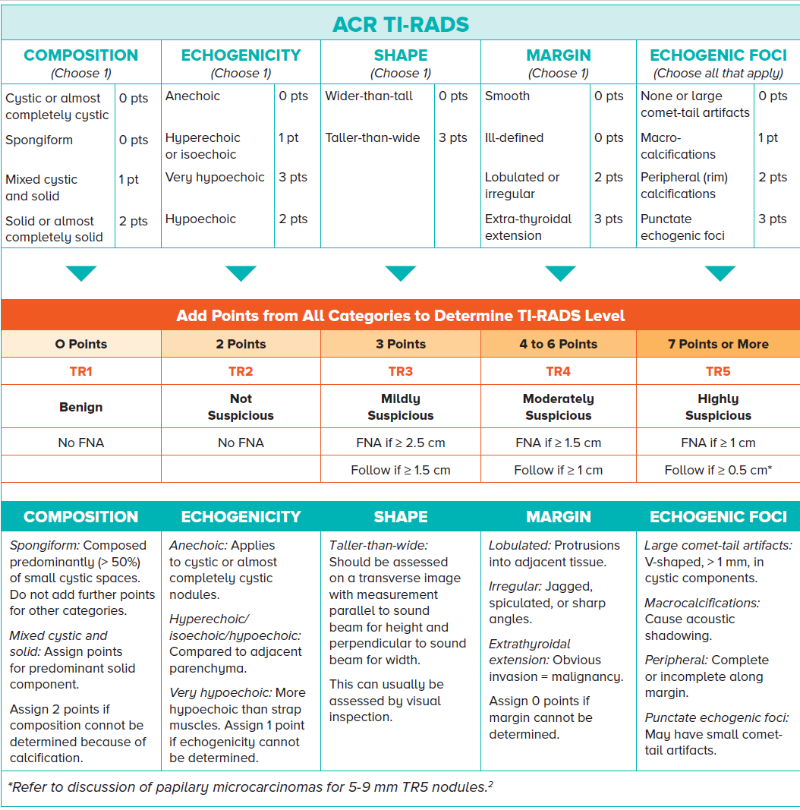
Figure 2
3. Fine needle aspiration cytology
When it is needed
The introduction of TI-RADS in thyroid sonography
has provided a standardised and objective tool
for thyroid nodule assessment, thereby reducing
ambiguity around which nodules require cytologic
evaluation.
Suspicious nodules are further investigated with
fine needle aspiration cytology (FNAC).
Procedure and reporting
In this procedure, which can be US-guided, a
needle is introduced into the nodule to collect
cells. This is generally a safe procedure and can
be performed as day surgery.
The FNAC results will then be reported by the
pathologists using the Bethesda system3 (Figure
3), which estimates a higher risk of malignancy
with corresponding higher Bethesda grading.
This then provides the attending clinician with a guide for counselling the patient regarding the
management options and recommendations.
Nondiagnostic/unsatisfactory -
Cyst fluid only
- Acellular specimen
- Other: Obscuring factors
| 5 - 10% | 5 - 10% | Repeat FNA under
US guidance |
Benign -
Benign follicular nodule
- Chronic lymphocytic (Hashimoto) thyroiditis, in proper clinical setting
- Granulomatous (subacute) thyroiditis
| 0 - 3% | 0 - 3% | Clinical and US follow-up until two negative |
| Atypia of undetermined significance /
follicular lesion of undetermined significance | 6 - 18% | 10 - 30% | Repeat FNA, molecular testing or lobectomy |
| Follicular neoplasm / suspicious for a follicular neoplasm (Specify if Hurthle cell type) | 10 - 40% | 25 - 40% | Molecular testing,
lobectomy |
| Suspicious for malignancy | 45 - 60% | 50 - 75% | Lobectomy or near-total thyroidectomy |
Malignant - Papillary thyroid carcinoma
- Medullary thyroid carcinoma
- Poorly differentiated carcinoma
- Undifferentiated (anaplastic) carcinoma
- Squamous cell carcinoma
- Carcinoma with mixed features
- Metastatic malignancy
- Non-Hodgkin lymphoma
- Other
| 94 - 96% | 97 - 99% | Lobectomy or near-total thyroidectomy |
Figure 3 2017 Bethesda System for Reporting Thyroid Cytopathology
NIFTP: Non-invasive follicular thyroid neoplasm
MANAGEMENT OPTIONS
1. Ultrasound surveillance
As the majority of thyroid nodules are benign
and indolent, and do not cause symptoms, they
can generally be monitored with US surveillance. These include:
- TR3-5 nodules that may not meet the size
criteria for FNAC
- FNAC-proven benign nodules and for which
patients are asymptomatic
Follow-up screening recommendations
As the risk of malignancy increases with higher
TI-RADS grading, the recommended frequency of
performing US thyroid surveillance is as follows:
TR1-2 nodule: US surveillance is not routinely
required, especially for asymptomatic patients.
Patients may be advised to observe themselves
and return if symptomatic.
TR3 nodule: Follow-up at 1, 3 and 5 years
TR4 nodule: Follow-up at 1, 2, 3 and 5 years
TR5 nodule: Annual follow-up till 5 years
2. Surgery
Thyroidectomy is a common and generally safe
head and neck surgical procedure and may be
indicated for some patients who present with
thyroid nodules or goitres.
The extent of surgery will either be a hemithyroidectomy
(lobectomy) or a total thyroidectomy.
In addition, for cancer cases, additional surgical
procedures may be performed as indicated (e.g.,
neck dissection for lymph node clearance).
Indications
The indications for surgery are:
- Proven or suspected thyroid malignancy
- Benign nodules/goitres causing compressive
symptoms
- Thyrotoxicosis resistant to medical therapy
- Patient preference
Surgical methods
a. Traditional neck incision
The majority of thyroidectomies are performed
via the traditional neck (transcervical) incision.
This surgical approach is well-established and
provides the most direct access to the thyroid
gland, thereby allowing safe instrumentation to remove the thyroid gland while preserving
vital adjacent structures such as the recurrent
laryngeal nerve and the parathyroid glands.
Although this approach invariably requires a
neck scar, the majority of cases heal very well
and are usually not conspicuous with time.
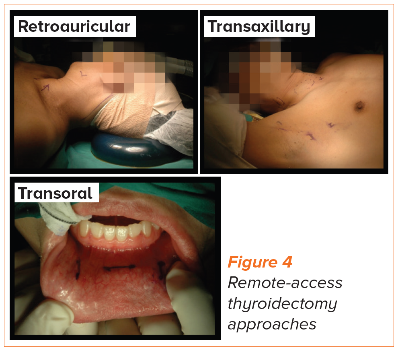
b. Remote-access procedures
Remote-access approaches (e.g., transaxillary,
retroauricular or transoral approaches) avoid
an anterior neck scar but surgical access to the
thyroid gland is not as direct, requiring a wider
extent of dissection and longer operative times.
These approaches may not be suitable for
certain patients such as those with larger
nodules/goitres or thyroid malignancy. Careful
patient selection with thorough counselling is
therefore imperative for patients who may be
keen on these remote-access procedures.
3. Thyroid nodule ablation
Thyroid ablation, first introduced in Singapore in
2017, has been shown to be effective in treating
symptomatic benign thyroid nodules.
This procedure involves introducing a small probe
into the nodule, after which heat is generated to
ablate (or destroy) the tumour. Size reduction of
the nodule then takes place slowly over months.
The most common technology used is that of
radiofrequency ablation (RFA). It is minimally
invasive, can be performed as day surgery and is
shown to be effective in shrinking benign nodules.
Selected patients with small papillary thyroid cancers who cannot undergo surgery may also be
candidates for thyroid nodule ablation.
Thyroid nodules are very common, and there
currently are guidelines in place within
SingHealth institutions for the attending physicians
to manage them in a timely and safe
manner. What GPs can do
Many of these patients can be monitored in
the primary care setting, typically those who
are asymptomatic with nodules that have been
assessed to be benign (TR1-2, FNAC-proven) or
have been stable on serial US. When to refer to a specialist
Indications for referral to specialist care will
include: - Patients who are symptomatic or have
red flag features
- Larger nodules (> 4 cm)
- Increase in size of nodules during
surveillance (> 20% increase in two
dimensions)
|
REFERENCES
2015 American Thyroid Association Management Guidelines
for Adult Patients with Thyroid Nodules and Differentiated
Thyroid Cancer.
Tessler FN, et al. ACR Thyroid Imaging, Reporting and
Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. Journal of the American College of Radiology. 2017
May;14(5):587–959.
Ali SZ, Cibas ES. The Bethesda System for Reporting Thyroid
Cytopathology, 2nd ed. Cham, Switzerland: Springer; 2017.
Dr Too Chow Wei graduated from the Faculty of Medicine, National University of Singapore
in 2003. He subsequently trained at various hospitals in Singapore in the diagnostic
radiology training programme and attained specialisation accreditation in 2012.
He is currently a Senior Consultant at the Department of Vascular and Interventional
Radiology and the Director of Interventional Services at Singapore General Hospital. He
has a keen interest in the realm of interventional oncology and palliation, with experience
in the ablation of liver, lung, kidney and bone tumours.
Dr Tay Ze Yun graduated from the National University of Singapore and received his
medical degree from the Yong Loo Lin School of Medicine in 2008. He subsequently joined
the SingHealth Otolaryngology Residency Programme as part of the inaugural batch of
residents and completed his specialist training in 2016.
In pursuit of his sub-speciality interest in head and neck surgery, he completed the two-year
SingHealth Duke-NUS Head & Neck Centre Fellowship Programme (2016-2018).
He was subsequently awarded the Ministry of Health’s Health Manpower Development
Plan award in 2018 to pursue a surgical fellowship in advanced head and neck surgical oncology at the world-renown Chang Gung Memorial Hospital in Taiwan.
Dr Tay also completed the International Federation of Head and Neck Oncologic
Societies fellowship and graduated with honours in 2020. He is currently a Consultant at
the Departments of Otorhinolaryngology –Head & Neck Surgery at Sengkang General
Hospital and Singapore General Hospital.
GPs can call the SingHealth Duke-NUS Head & Neck Centre for appointments at the following hotlines:
Singapore General Hospital: 6326 6060
Changi General Hospital: 6788 3003
Sengkang General Hospital: 6930 6000
KK Women’s and Children’s Hospital: 6692 2984
National Cancer Centre Singapore: 6436 8288
National Dental Centre Singapore: 6324 8798
