Mr Ramasamy Sinnasamy, 61, was diagnosed with Chronic Obstructive Pulmonary Disease. Thanks to the multidisciplinary care at the SingHealth Duke-NUS Lung Centre, he is now back to work and enjoying family time.
Mr Ramasamy Sinnasamy, 61, was diagnosed with Chronic Obstructive Pulmonary Disease. Thanks to the multidisciplinary care at the SingHealth Duke-NUS Lung Centre, he is now back to work and enjoying family time.
Mr Ramasamy Sinnasamy, 61, teared up as he recalled his near-death experience when he was admitted to hospital in 2014. “When I left the hospital to return home, the doctors told me I had been given a second life.”
Mr Ramasamy had a persistent cough for four months when he decided to visit the polyclinic for a check-up. At the clinic, he started feeling breathless and was sent to the hospital immediately, where doctors diagnosed him with Chronic Obstructive Pulmonary Disease (COPD). His condition was so severe that he had to stay in the Critical Care Unit. “With all the panic and uncertainty, we were so scared. We feared the worst,” shared his wife, Mdm Sarasvathy.

Upon discharge, the loving husband and doting father of three daughters, worked hard to get his life back on track. With his wife and daughters as his motivation, he promptly adopted healthier dietary habits and gave up smoking. “I remember when my father was admitted, his very first thoughts were on how his girls – my mother and my sisters, were faring,” recalled his eldest daughter, Shanthini, 26, “We were the reason he kept fighting.”
Despite his best efforts, Mr Ramasamy was admitted to hospital again in August 2017 for COPD exacerbation and anaemia.
The human touch

Thanks to the excellent care by the team at Singapore General Hospital (SGH), Mr Ramasamy’s condition has since stabilised and he is back to working full-time as a coach driver. He visits the SingHealth Duke-NUS Lung Centre, a SingHealth Duke-NUS Disease Centre (SDDC), every four to six months, where he is under the care of Dr Jessica Tan Han Ying, a Consultant at the Lung SDDC, and Ms Lee Siew Ling, a Nurse Clinician.
Siew Ling helps monitor Mr Ramasamy’s condition and teaches him how to keep his condition under control. She also followed-up with phone calls, to ensure that he was coping well. “He is a very good patient. COPD is a progressive disease, so making lifestyle changes and being able to independently manage his medication is important. Mr Ramasamy is very willing to follow our advice closely.”
Over the years, Mr Ramasamy and Dr Tan have developed a strong bond. “She has helped me a lot. She listens and addresses my concerns, and always patiently assures me. She is meticulous and really cares for her patients,” he smiled.
Dr Tan shared a memorable moment when she visited Mr Ramasamy in hospital last August. “His eldest daughter called and asked if I could visit him in the ward. He was in distress, but calmed down when I spoke to him and assured him that he was in good hands. It was very heart-warming because he was just happy to see me. This is the kind of trust-based relationship that we try to build with our patients.”

Integrated model of care
COPD affects more than just the lungs and can impact patients’ ability to work, sleep, go about their daily routine and their mental wellbeing. The COPD integrated clinic at the Lung Centre provides care in every aspect.
“We all work as a team. At the Lung Centre, doctors, nurses and allied health professionals come together to ensure that the patient has seamless care,” explained Siew Ling. This integrated model of care has benefitted Mr Ramasamy and other COPD patients – they get a one-stop access to lab tests, consultation with lung specialists and surgeons, physiotherapy, patient education by nurses and support of medical social workers.
A patient turn advocate
Four years from when he was first diagnosed with COPD, Mr Ramasamy lives life positively and has even taken the step to get actively involved in research trials. Spurred on by his family, he is an ambassador for smoking cessation, encouraging newly-diagnosed patients who are trying to quit. He tells them, “Don’t go to the doctor too late. See the doctor, get treated early and make sure you follow the advice.”

Mr Ramasamy's journey was facilitated by the SingHealth Duke-NUS Lung Centre, a SingHealth Duke-NUS Disease Centre (SDDC). Read about the journeys of our patients' success stories in our latest annual report.
| SingHealth Duke-NUS Disease Centres What are SDDCs?
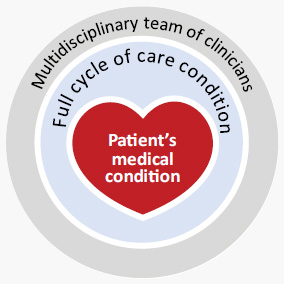 SingHealth Duke-NUS Disease Centres (SDDCs) were formed as a strategic model of care for patients with specific conditions that require multi-disciplinary teamwork. The structure enables professionals from different disciplines and institutions to work closely together to enhance care. SDDCs provide quality clinical care throughout the care continuum and improve outcomes. In conventional care, a patient with a nodule (growth of abnormal tissue) in his neck may be referred to a thyroid specialist or surgeon, who would then refer him to a diagnostic radiologist for imaging tests. If the nodule is found to be a cyst, the patient would be given an appointment for a biopsy. By this time, the patient would have made multiple trips to the hospital to see different specialists.With the SDDCs, the patient’s journey is streamlined, cutting down the number of visits, saving time and money. It also translates to greater work efficiency for clinicians. For tomorrow’s medicine
SDDCs’ approach to collaborative care places emphasis on developing a comprehensive database for care and research. In the long term, it will change the way we recommend treatments – as outcomes are collectively measured and studied to continuously improve protocols. 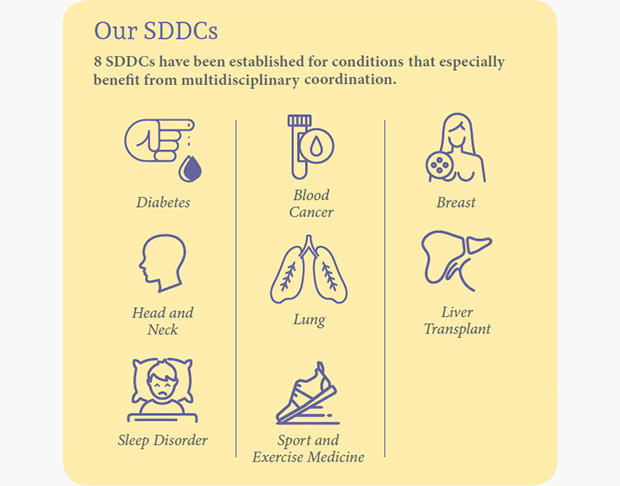
|

