The 'three highs' - high blood pressure, high blood sugar, and high cholesterol – are well
known health concerns. Learn more from National Heart Centre Singapore (NHCS) Murmurs article.
The 'three highs' - high blood pressure, high blood sugar, and high cholesterol – are well known health concerns. However, few people realise that these conditions often occur together, alongside excess body fat around the waist. When combined, they form a cluster known as metabolic syndrome, which is becoming increasingly common in Singapore.
By Dr Ruan XuCong, Associate Consultant, Department of Cardiology
Metabolic syndrome is not a single disease, but rather a combination of interrelated health problems.
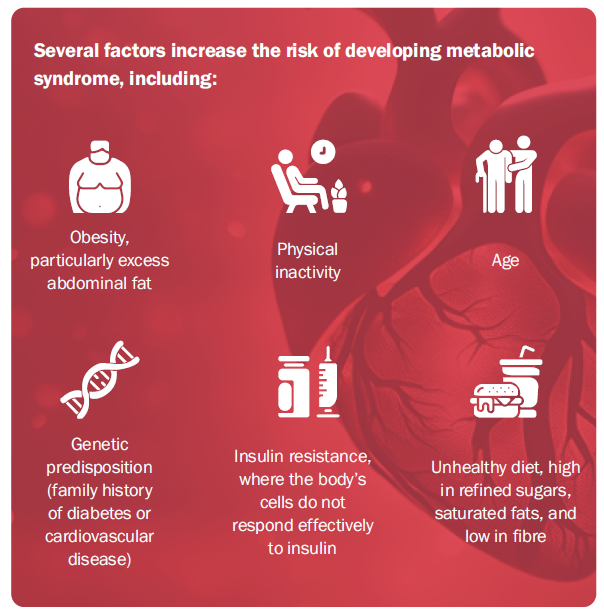
This grouping significantly increases one’s risk of heart disease, stroke, and other serious issues. It is a serious and growing public health concern, driven largely by lifestyle factors such as poor diet, physical inactivity, and rising obesity rates.
Globally, metabolic syndrome affects approximately 25% of adults1. Its prevalence is on the rise, fuelled by obesity and sedentary lifestyles. In the U.S., about 40% of adults above the age of 60 years old have metabolic syndrome2. Singapore also reports increasing rates over the years. With rising obesity rates in Asia and worldwide, metabolic syndrome poses an increasing burden on healthcare systems due to its association with long-term health complications.
Metabolic syndrome is diagnosed when a person has at least three of the following symptoms and signs3:
High waist circumference
| Asian men: ≥ 90cm
Asian women: ≥ 80cm
|
High blood pressure
| ≥ 130/85 mmHg
|
Elevated fasting blood sugar
| ≥ 5.6 mmol/L
|
High triglycerides
| ≥ 1.7 mmol/L
|
Low HDL cholesterol levels
| Men: < 1 mmol/L
Women: < 1.3 mmol/L
|
It is worth noting that some people may not show any symptoms, particularly in the early stages, which underscores the importance of regular health screenings. In many cases, metabolic syndrome is diagnosed during routine check-ups. Given its often silent nature, it is not surprising that metabolic syndrome is frequently misunderstood. To clear up some common misconceptions:
“Only overweight individuals are at risk.”
This is not true. While excess weight increases the risk, even thin individuals with poor diets or sedentary lifestyles can develop metabolic syndrome.
“It’s not serious.”
In fact, metabolic syndrome is linked to severe long-term health risks if left unmanaged.'
“Medication alone can manage the condition.”
While medication can help, lifestyle changes are crucial for long-term management and prevention of metabolic syndrome.
Lifestyle plays a crucial role in both preventing and managing metabolic syndrome. A healthy diet low in refined sugars and saturated fats, while rich in fruits, vegetables, whole grains, and lean proteins, can help control blood sugar and cholesterol levels. Regular exercise aiming for at least 150 minutes of moderate activity weekly can reduce insulin resistance, improve blood pressure, and support weight loss. Even modest weight loss can significantly lower risks. Lastly, refrain from smoking and limit alcohol intake as these habits can contribute to the development of metabolic syndrome.
Treatment often involves a combination of medications and lifestyle changes. Some common medications include those for blood pressure control, statins to lower cholesterol, and diabetes medication to manage blood glucose. However, medication alone is not sufficient. Sustainable lifestyle changes are crucial for long-term management and prevention.
If left untreated, metabolic syndrome can lead to severe health issues such as cardiovascular disease (e.g., heart attack, stroke), fatty liver disease, and chronic kidney disease.
For individuals already diagnosed with metabolic syndrome, regular monitoring of blood pressure, glucose levels, and cholesterol is essential. A personalised care plan with healthcare providers, including doctors, dietitians and physiotherapists, can minimise risks and prevent complications.
Overall, metabolic syndrome is preventable and manageable, with lifestyle adjustments serving as the cornerstone of both prevention and treatment.
REFERENCES
1. O’Neill, S. & O’Driscoll, L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obesity Reviews 16, 1–12 (2015).
2. Cho, L. W. Metabolic syndrome. Singapore Med J 52, 779–785 (2011).
3. Grundy, S. M. et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 112, 2735–2752 (2005).
This article is from Murmurs Issue 48. Click here to read other articles or issues.
