Assistant Nurse Manager Lui Kok Wah, seen here with a mock patient, is a member of a teamlet of doctors and nurses. Polyclinic patients with predefined chronic conditions, are matched to teamlets at SHP, and at consultations will see the same teamlet members.
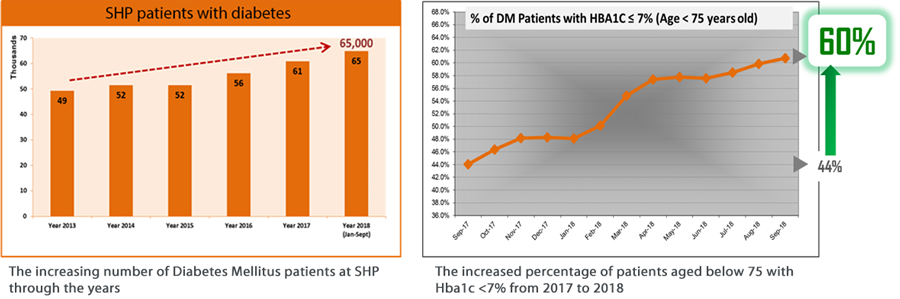
SingHealth Polyclinics, which has handled more diabetic patients year on year, has seen an increased number of them gaining good control of their condition. Here’s why.
In 2017, about half of the diabetic patients managed at SingHealth Polyclinics (SHP) aged below 75, gained very good control of the disease.
Forty-four per cent of them had an hbA1c level (the measurement of red blood cells coated with sugar) below 7, a target level set for diabetic patients in 2017. This figure showed a further increase to 60 per cent towards the end of 2018.
Prescribing new drugs
According to Dr Gilbert Tan, Director, Clinical Development & Integration, SHP, the good outcomes were the result of many factors, including the availability of two new oral drugs to treat diabetes in SHP.
The drugs - Dapagliflozin and Empagliflozin - belong to a class of diabetes medication known as sodium-glucose cotransporter-2 (SGLT-2) inhibitors. They add to the collection of drugs for diabetic patients with suboptimal control who are not ready to accept insulin therapy.
The new drugs work differently from other diabetic drugs, and represent an added option in the battle against diabetes.
Dr Tan said that the drugs have advantages such as not causing weight gain, well tolerated and rarely cause hypoglycaemia (low blood sugar). They lower HbA1c by 0.5% to 0.8%. He stated that with every drop in the level of hbA1c, there will be a reduction of complications associated with diabetic microvascular problems, such as diabetic retinopathy, bleeding in the eye, and kidney injury. In addition, optimal control of diabetes will reduce the risks of heart attacks and deaths from diabetes.
“Some patients respond better to these new drugs. However, although the drugs help to sustain their condition before the need to move to insulin, ultimately, oral drugs cannot replace insulin therapy,” said Dr Tan

Dr Gilbert Tan says the new drugs represent an added option in the battle against diabetes.
Teamlets and care paths
Another reason for the better outcomes was the formation of new teamlets and care paths at SHP.
“In earlier years, patients were not matched to the same care team, hence there were no proper follow-up visits on their conditions. Currently, patients with predefined chronic conditions are enrolled into our teamlets, which consist of doctors, and care managers (nurses trained in chronic disease management) who they will see on a regular basis,” said Dr Tan.
In 2018, SHP also developed standardised care paths for newly diagnosed diabetic and pre-diabetic patients, where they are referred to the same care team for structured management, counselling and reviews.
“We found that through the use of care paths, patients knew more about their own condition and were more confident of managing it themselves. Pre-diabetic patients were also looped into this care, because we should intervene at the pre-diabetes stage to reduce their risk of developing diabetes later on,” said Dr Tan.
Building patient awareness – an ongoing task
Patient-empowerment was also a reason for the improvement. With awareness, patients are more motivated to take control of their glucose levels.
Dr Tan emphasised that patient-education is not a new strategy, but an ongoing effort by SHP to empower patients to take control of their health conditions. The continuous efforts to create awareness in the public has been done through community events, such as health talks, exercise programmes, cooking demonstrations and healthy eating tips during festivals.
Moving forward
Dr Tan said SHP will continue to track the progress of its teamlets to review its effectiveness. The aim is to promote better self-care by empowering patients to properly monitor their blood sugar levels and insulin dosages.
Patients may ultimately be directed to remote consultations with nurses through telecare. Those referred for telecare will get regular phone support by telecarers, who are experienced and trained nurses. They support diabetic patients with knowledge and skills to manage their condition confidently at home.
SHP is also working beyond delivering care in the clinics, and collaborating with community partners to manage complex patients with medical and social needs.
A pilot project previously conducted using geo-spatial mapping (like finding dengue hotspots) identified a cluster of patients with poor diabetic control, many of whom were living in blocks of one-room flats around the Marine Parade area. They had been diagnosed with diabetes previously but had not returned for follow-up treatment.
“Patients such as those in this group often cannot afford fresh meals, and subsist on canned food or instant noodles. We are in the process of scaling this up, to play our part by connecting them to social networks for assistance.” said Dr Tan.
