The universal Lynch Syndrome Screening Programme at KKH is changing the lives of women.
By Dr Adele Wong, Ms Eliza Courtney and Dr Joanne Ngeow
An inherited disorder, Lynch syndrome causes patients to have a higher lifetime risk of developing colorectal cancer (31-38%), endometrial cancer (33%), ovarian cancer (9%) as well as other malignancies.
Also known as hereditary non polyposis colorectal cancer, the condition has an estimated incidence of between 1 in 300 and 1 in 500 in the general population. Endometrial cancer is particularly prevalent in women with Lynch syndrome.
Previously, patients with Lynch syndrome were identified clinically using validated criteria followed by confirmatory gene testing. Unfortunately, the majority of endometrial cancer patients with Lynch syndrome did not meet the criteria due to an absence of personal or family history suggestive of the condition. As such, laboratory-based tests are critical to any Lynch syndrome screening programme.
By diagnosing the condition early, endometrial cancer patients with Lynch syndrome can be given timely and appropriate management to help reduce the potential of a second tumour.
To enable early diagnosis of Lynch syndrome, in February 2017, KK Women's and Children's Hospital (KKH) established a universal Lynch Syndrome Screening Programme for all patients diagnosed with endometrial cancer, regardless of age, based on the recommendation by the Society of Gynaecologic Oncology.
The KKH universal Lynch syndrome screening pathway starts with laboratory-based immunohistochemistry (IHC) staining and microsatellite instability (MSI) analysis on the tumour tissue. The two tests determine if the patient has mutations in the genes associated with Lynch syndrome.
Patients with positive results are referred to National Cancer Centre Singapore (NCCS) for further clinical examination, work-up and counselling. Finally, a germline gene analysis is performed to confirm the Lynch syndrome diagnosis.
By diagnosing the condition early, endometrial cancer patients with Lynch syndrome can be given timely and appropriate management to help reduce the potential of a second tumour. For her relatives, appropriate tumour surveillance may prevent cancers through timely identification of lesions at the pre-malignant stage.
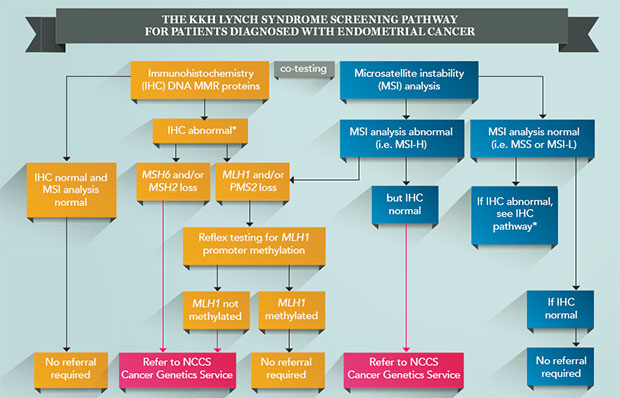
All patients diagnosed with endometrial cancer at KKH will be screened for Lynch syndrome, regardless of age. As the IHC and MSI screening tests do not distinguish between somatic and germline mutations in the DNA MMR genes, conformational germline gene analysis will be performed after further clinical examination, work up and appropriate counselling.
A KKH patient, 57-year-old Madam Tan (not her real name), was diagnosed with endometrial cancer and underwent surgery. Post-procedure, in line with the new screening pathway, her doctors screened her for Lynch syndrome. Her IHC and MSI results indicated that she had a genetic mutation associated with Lynch syndrome.
While undergoing chemotherapy at KKH, Madam Tan was concurrently referred to receive genetic counselling at the National Cancer Centre Singapore (NCCS) based on her results. She was surprised at her referral, as she was unaware of any family history of cancer, apart from her paternal aunt being diagnosed with colon cancer two decades prior.
Through genetic counselling, she discovered family history consistent with Lynch syndrome involving her paternal grandfather and his two siblings. Genetic testing also confirmed her Lynch syndrome diagnosis.
Her children were diagnosed with the condition as well, and they started going for annual colonoscopies to catch signs of cancer early.
When possible, universal screening should be done to supplement reported family history, as it is beneficial in identifying patients who are likely to suffer from Lynch syndrome. In addition, a multidisciplinary approach to the care management of these patients and their families is crucial.
In Madam Tan's case, her diagnosis and the establishment of a detailed genetic family tree will help future generations in her family receive appropriate counselling and take precautionary steps by undergoing regular cancer screening when required.
This article is an extract from "Saving Lives, Changing Futures", first published in the KKH publication Special Delivery Vol 66, Issue 1. To read the full article and find out more details about the programme described, click here.
 | Dr Adele Wong,
Consultant, Department of Pathology and Laboratory Medicine, KK Women's and Children's Hospital and Adjunct Instructor, Pathology Academic Clinical Program, Duke-NUS Graduate Medical School Singapore.
Dr Wong underwent a fellowship in gynaecologic and breast pathology at Massachusetts General Hospital, Boston, USA, as part of the SingHealth Health Manpower Development Plan in 2015. Her research interests include gynaecological pathology, in particular endometrial carcinomas. |
 | Ms Eliza Courtney,
Genetic Counsellor, Cancer Genetics Service, Division of Medical Oncology, National Cancer Centre Singapore.
Ms Courtney delivers genetic counselling services regarding hereditary cancer syndromes to patients with cancer and their families. She holds a Masters of Genetic Counselling from the University of Sydney, Australia, and has previously held genetic counselling positions at a number of tertiary hospitals in Sydney. |
 | Dr Joanne Ngeow,
Head, Cancer Genetics Service, National Cancer Centre Singapore and Assistant Professor, Oncology Academic Clinical Program, Duke-NUS Graduate Medical School.
Dr Ngeow currently leads the Cancer Genetics Service at NCCS with an academic interest in hereditary cancer syndromes and translational clinical cancer genomics. Her current clinical focus and research revolves around understanding cancer predisposition by studying cancers clustering in families, young adults and in families with multiple / rare cancer presentations. |
