The HEARTS team explored various methods that could improve specimen collection and deployed four solutions over the span of four months to test out the effectiveness.
HEARTS Team (L-R): Senior Staff Nurse (SSN) Jubinal Geraldine 44-HD; Assistant Nurse Clinician (ANC) Koh Hwee Hong, Ward 44-CCU; NC Low Huiling, Ward 44-CCU, co-leader; NC Belinda Wong, Ward 44, leader; and Lay Sock Yee and Jacqueline Huo from Quality Management. (Not pictured: SNM Jasmine Lee, Ward 44-CCU, facilitator; SSN Nuraishah Binte Ali Hassan, Ward 44-ICA; NC Sun Xia, Ward 44; ANC Luo Tao, Ward 44-ICA; and Kelvin Tiong, Division of Pathology, SGH).
92 minutes.
That was how long it took to do a full blood test in the ward, a process that involves multiple parties from placing of a blood test order by a doctor, collecting and dispatching blood specimen by a nurse, to eventually receiving a successful result from the laboratory staff.
What if something goes wrong along the way and the specimen collected is rejected? “Another 145 minutes is needed to repeat the entire process which leads to our nurses spending lesser time on bedside patient care,” said Nurse Clinician (NC) Belinda Wong, Ward 47B, leader of quality improvement team, HEARTS team.
More importantly, a rejected blood specimen would cause a delay in treatment, increase the medical costs for the patient, and subject him or her to another round of blood taking, a process that may be unpleasant for some patients.
The problem
The team first noticed an upward trend of rejected specimens in 2018 with an average rejected specimen rate of 0.95%. They discovered the top reasons for rejected specimen – 32% due to insufficient specimen (i.e. insufficient blood), 17% due to leakage, and another 17% due to clotted specimen.
“Through our analysis, we realised that the rejected specimen came about due to a lack of experience in performing venepuncture and staff being unfamiliar with the different requirements, such as the amount needed and sequence of each specimen tube,” shared co-leader, NC Low Huiling, Ward 44.
Meeting the target with four solutions
The team explored various methods that could improve specimen collection and decided to deploy four solutions over the span of four months to test out the effectiveness.
Visual guidance
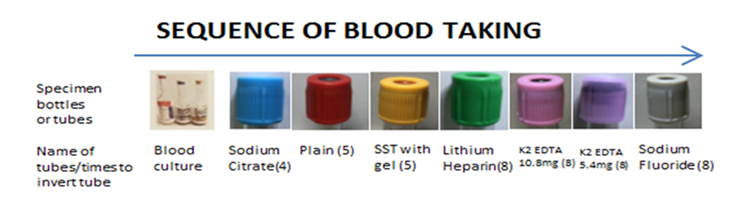
A simplified visual aid on the correct sequence of blood taking was placed above monitors on the Computer-on-Wheels (COWs) to remind and guide staff on the amount of blood needed during blood collection.

In addition, a set of samples displaying the actual amount of blood required per tube was placed at the pneumatic tube area for staff to counter check before they send the specimens to the laboratory.
Re-educate through roadshows and meetings

Refresher workshops and meetings were conducted to educate staff on specimen collection practices, and to reinforce the need to adhere to the correct and effective methods of specimen collection. Weekly data on the trends of rejected specimen was also collected and communicated during roll calls.
24-hour Phlebotomist

To standardise the blood taking process, the team implemented a 24-hour Phlebotomist to take all blood specimens. Patient Care Assistants (PCAs) were called upon to take on the expanded role through comprehensive training. “I feel more confident with my new role and patients now call me the ‘vampire’!” shared PCA Hazel Cataraquit. To reinforce this measure, the mobile contact number of the Phlebotomist on duty was displayed at every nurse station for staff to contact easily.
Additional check point

A basket to collect swabs was placed at every nurse station for the Patient Service Assistant to ensure that the caps on the tubes are closed tightly with no leakage before they are despatched.
The golden results
With the new work processes in place, the team saw a significant drop in rejected specimen almost immediately. The average rejected specimen rate spanned across the four months of implementation was around 0.6%, well meeting the team’s target of below 0.7%.
“The effective workarounds not only increased the productivity of the staff, saved time and costs, but also enhanced patients’ safety and experience. The project was so successful that the initiatives were also rolled out across all NHCS inpatient wards and shared with other institutions’ wards,” beamed NC Wong.
To top it off, the HEARTS team clinched the Gold Award at the Team Excellence Symposium 2019, part of the Innovation & Quality Circles (IQC) movement organised by the Singapore Productivity Association.
