NCSE are seizures in critically ill, comatose patient. Important to recognise it in a timely manner. Treat NCSE as quickly as possible but with minimal use of sedatives and anaesthetics, to avoid prolonging the coma and intubation.
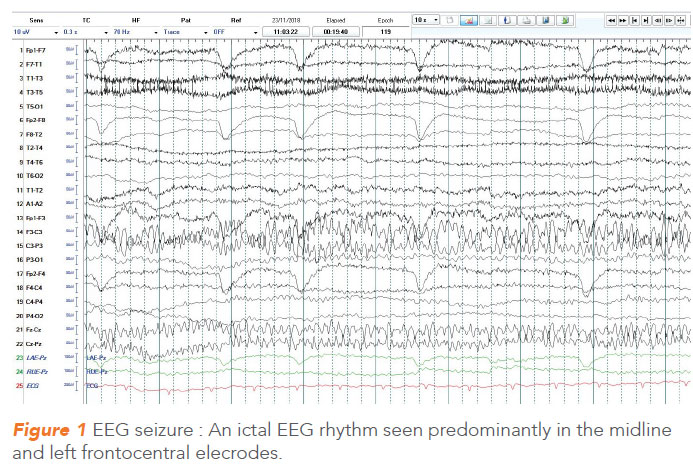
Non-convulsive status epilepticus (NCSE) is an under-recognised form of status epilepticus characterised by absence of motor manifestations of seizures in the presence of an ictal EEG rhythm (Figure 1). Thus, NCSE is essentially an electroencephalographic (EEG) diagnosis, and is characterised by lack of the classical clinical manifestations of convulsive seizures. It can be seen in a myriad of clinical situations, but the prototypical NCSE as discussed occurs in the setting of critically ill, comatose or stuporous patient in an intensive care unit.
The other situations where NCSE occurs include:
(a) after a convulsive seizure
(b) In a patient with chronic epilepsy (focal or generalised)
The diagnosis is often not straight forward and the most important variables contributing to the diagnostic dilemma are the clinical setting in which it occurs and the haziness in defining what EEG rhythm constitutes an ictal EEG.
BACKGROUND
Back in the 19th century, before EEGs were developed, prolonged confusional states were thought to be seizures.
In the 1940s, the EEG was introduced. In 1956, Gastaut first described a case of psychomotor status – a type of status epilepticus associated with altered mental state which could be similar to NCSE.
NCSE is now gaining increasing attention. Diagnosis is based on ictal EEG pattern, together with altered mental state. Response to antiepileptic drugs (both clinical and EEG improvement) is often included in the criteria for its diagnosis.
HOW COMMON IS THE PROBLEM?
The incidence of NCSE differs in reported studies. This is particularly due to the differences in the baseline characteristics of the populations studied. In comatose or obtunded, critically ill patients, the incidence of NCSE ranges from about 8% to 27%. In 2000, Towne et al.1, studied 236 comatose patients who underwent EEG for coma evaluation, and found that 8% of those patients had NCSE. In 2004, Claassen et al.2 reported 570 critically ill patients with unexplained decreased level of consciousness. These patients underwent continuous EEG (CEEG) monitoring and 19% of them had seizures that were almost always non-convulsive in nature. Westover et al.3 reported 27% seizure occurrence in a cohort of 625 acutely ill hospitalised adults. Thus, the problem of NCSE is real and significant in critically ill patients.
DECIDING BETWEEN ROUTINE EEG OR CONTINUOUS EEG FOR DIAGNOSIS
NCSE, particularly if prolonged, has potential to cause secondary neuronal injury. Hence it is important to recognise it in a timely manner. Since seizures are intermittent, an important question is whether a conventional half an hour duration EEG would be enough to confirm the diagnosis of NCSE.
It is known that CEEG monitoring is very likely to give a higher diagnostic yield as compared to routine EEGs. Sutter et al.4 compared patients with suspected NCSE who underwent routine and continuous EEG monitoring and found a significantly high NCSE detection rate with CEEG.
Therefore, despite the fact that continuous EEG is labour intensive and costly, it should be considered whenever it is feasible, when NCSE is in question. This is particularly true in high risk patients for NCSE, which include :
(a) patients who have had a generalised tonic-clonic seizure (GTCS) episode and continue to be obtunded beyond the expected postictal period
(b) patients with supratentorial brain injury with unexplained encephalopathy
(c) patients with sepsis and multi-organ failure with encephalopathy
(d) patients with refractory status epilepticus on weaning doses of anaesthetic agents, and
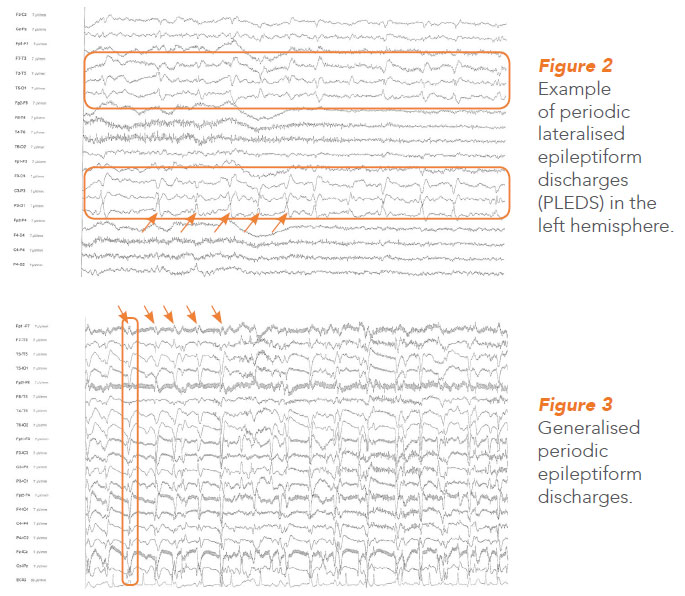
(e) patients who are found to have periodic lateralised epileptiform discharges (PLEDS) (Figure 2 ) or generalised periodic epileptiform discharges (GPEDS) (Figure 3 ) on routine EEG
LENGTH OF MONITORING
Once CEEG is initiated, the next step is to determine the duration of monitoring. There is evidence to suggest that seizure risk in acute neurologic illness reduces rapidly with time, and hence a substantial risk stratification is possible based on early EEG abnormalities.
About half of the seizures are recorded within the first hour itself, and by 24 hours, about 90% of seizures would be detected.
Interestingly, the first four hours of CEEG gives a valuable clue.
In one study, when there was no epileptiform activity seen in first 4 hours, none of those patients went on to develop NCSE during further CEEG monitoring5.
Based on this evidence, we often recommend 24 hours of CEEG monitoring for patients with confirmed non-convulsive seizures or NCSE after reasonable seizure control. This is to ensure that patients are no longer in NCSE. The duration can be modified based on clinician decision after consideration of holistic patient situation.
If there is a clinical suspicion of NCSE in a comatose intensive care unit (ICU) patient or altered mental status (AMS) after witnessed clinical seizure – there should be monitoring with CEEG for 4 hours. Any patient who, on conventional EEG, or during the first 4 hours of CEEG recording, has epileptiform discharges (EDs), the monitoring should be extended for 24 hours. If no seizure is recorded during this interval, CEEG monitoring can stop.
DIFFICULTIES OF CEEG MONITORING
Limitations of CEEG monitoring include:
- labour intensiveness
- high cost incurred
- ability to deal with technical issues out of office hours, e.g. leads dropping off
- ICU setting itself where a patient is connected to various monitoring equipment, and CEEG adding a big bulk to it. This not only adds to artefacts which make EEG reading difficult but also places limitations on patient handling due to fear of dislodging of electrodes.
There are pitfalls related to the diagnosis of NCSE as well. Firstly, there is an element of subjectivity and hence a high inter-rater variability as to what EEG pattern is ictal (equivalent to EEG seizure).
Also, there is a controversial borderzone in the ictal – interictal EEG spectrum, which may be interpreted as seizures by some neurophysiologists but not by others. Uniform consensus criteria are being developed with the most recent being the Salzburg criteria6 for diagnosis of NCSE being widely used now.
HOW TO MANAGE PATIENTS WITH NCSE
Two important issues should be borne in mind when considering treatment of NCSE in a critically ill patient. Firstly, though NCSE has the potential to cause neuronal injury, it is probably not as damaging as convulsive status epilepticus. Secondly, overzealous treatment with anaesthetic agents like propofol and thiopentone are associated with complications.
A balanced approach is recommended, with the aim to diagnose and treat NCSE as quickly as possible but with minimal use of sedatives and anaesthetics, so as to avoid prolonging the coma and intubation.
For critically ill patients with NCSE due to systemic causes, it is advisable to use boluses of benzodiazepines together with parenteral antiepileptic drugs (AEDs) like phenytoin, valproic acid or levetiracetam as first line agents. If continuous infusion of anaesthetic agent is needed, intravenous (IV) benzodiazepines like midazolam infusion will be administered with careful hemodynamic monitoring. NCSE following a convulsive SE may need more aggressive treatment.
The cause of NCSE may not often be clear, and there could be multiple etiologies. When known, treating the cause of NCSE is of utmost importance.
NNI’S EXPERIENCE WITH NCSE
According to NNI’s figures on NCSE, a 3% incidence of NCSE amongst inpatient EEGs ordered was found. Amongst the 81 NCSE episodes recorded, primary neurological cause was seen in 36%. 19% had purely systemic cause and 44% had combined neurologic and systemic cause. Poor outcome defined as death or significant functional decline, was seen in nearly half of the patients.
OTHER LONG-TERM EEG MONITORING
CEEG monitoring is a form of long-term EEG monitoring mostly used for inpatients with suspicion of non-convulsive seizures, or for monitoring after or during status epilepticus.
At NNI
Apart from CEEG for NCSE and status epilepticus, NNI currently has a video EEG monitoring room, where healthcare professionals conduct long-term diagnostic EEG studies for characterisation of episodes of uncertain etiology and also for pre-surgical work up for epilepsy patients.
When a patient with epilepsy reports of episodes which are different from usual historical seizures, if any patient presents with spells of uncertain nature, or suspected non-epileptic attack disorder, they can be referred to NNI’s epilepsy clinic where specialists may consider long term video EEG monitoring for selected patients.
GPs can call for appointments through the GP Appointment Hotline 6330 6363 for more information about the department.
REFERENCES
1. Towne AR, Waterhouse EJ, Boggs JG, Garnett LK, Brown AJ, Smith JR, DeLorenzo RJ. Prevalence of non-convulsive status epilepticus in comatose patients. Neurology 2000;54(2):340-345.
2. Claassen J, Mayer SA, Kowalski RG, Emerson RG, Hirsch LJ. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology 2004;62:1743–1748
3. Westover MB, Shafi MM. Bianchi MT et al. The probability of seizures during EEG monitoring in critically ill adults. Clinical Neurophysiology 2015; 126: 463-471
4. Sutter R, Fuhr P, Grize L, Marsch S, Ruegg S. Continuous video-EEG monitoring increases detection rate of non convulsive status epilepticus in the ICU. Epilepsia 2011;52:453-457.
5. Shafi MM, Westover MB, Cole AJ, Kilbride RD, Hoch DB, Cash SS. Absence of early epileptiform abnormalities predicts lack of seizures on continuous EEG. Neurology 2012;79:1796-1801.
6. Lettinger M, Trinka E, Gardella E et al. Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol. 2016;15:1054-1062.
By:
Dr Gosavi Tushar Divakar is a Consultant from the Department of Neurology, at the National Neuroscience Institute (SGH Campus). He graduated from Mumbai University in India and completed his neurology training in Singapore at the NNI. He did a fellowship at the National Hospital for Neurology, London, UK in Epilepsy. His areas of interest includes managing complex epilepsy cases, long term electroencephalogram monitoring, status epilepticus and non-convulsive status epilepticus.
