By Annie Tan, Singapore Health
When surgery involving the thyroid gland is needed, surgeons often turn to the conventional method where a long cut is made across the front of the neck. This procedure leaves a disfiguring scar – a flaw that has become synonymous with thyroidectomy.
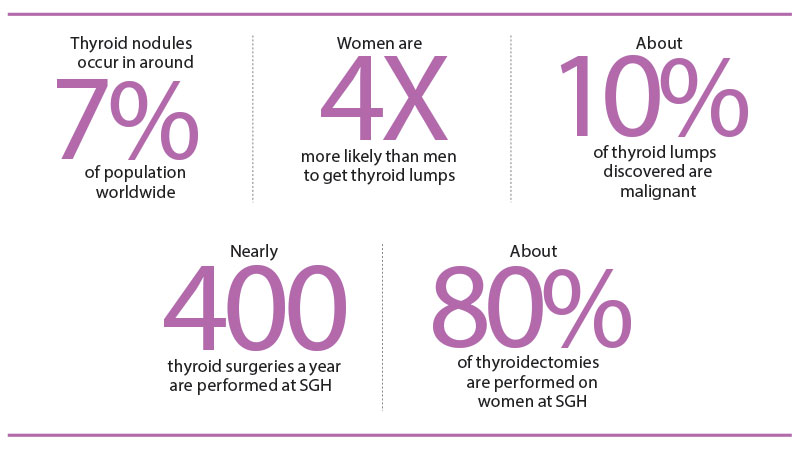
But a new surgical technique has become a viable alternative for patients, particularly women who are more prone than men to diseases of the thyroid, a butterfly-shaped gland at the front of the neck.
Known as transoral endoscopic thyroidectomy, the procedure involves a much smaller operating area – meaning patients experience less bleeding, less post-operative pain and quicker wound healing. Just as important, it leaves no visible scarring.
“A significant portion of my patients with thyroid lumps are young women in their prime. The anxiety they experience about the condition is often coupled with concerns about their cosmetic appearance after the operation to remove thyroid growth,” said Dr Jeremy Ng, Senior Consultant and Head, Department of General Surgery, Singapore General Hospital (SGH). He is also a member of the Duke-NUS Head and Neck Centre.
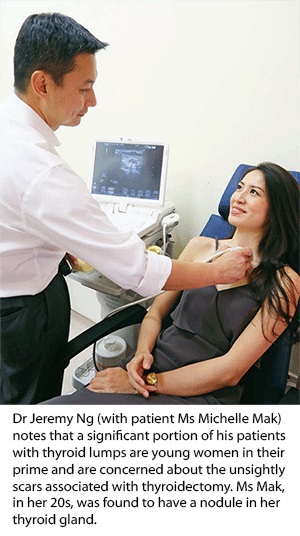
“The transoral approach affords a safe technique to remove these lumps, whether malignant or not, with the added advantage of not leaving behind a visible scar on the neck.”
The procedure makes three small incisions – 0.5cm to 10cm – in the lower lip, after which carbon dioxide gas is injected through the area to create a working space. A camera and endoscopic instruments are inserted through the holes, down the chin and neck to the thyroid gland. Scars behind the cuts heal are concealed in the lower lip.
The new procedure became available to SGH patients in December 2015, with 20 of them – all women – having undergone the surgery by April 2017. Following any thyroid surgery, patients experience hoarseness in their voice – often temporary – as the gland is near the voice box. They can also encounter difficulty swallowing, and numbness in the chin and neck, which ease when the swelling in the neck area subsides.
Depending on whether a partial or total thyroidectomy is done, blood calcium levels may also drop. This is because the four parathyroid glands – at the back of the thyroid – may be affected during surgery. The parathyroid glands produce hormones that regulate calcium levels in the body, while the thyroid gland produces hormones that regulate the body’s metabolism.
For all 20 patients, however, none experienced a voice change, and the four who had the entire thyroid gland removed didn’t have low calcium or excessive bleeding issues. Unless lumps are found on both sides of the thyroid, usually just half the gland is removed – partial thyroidectomy – leaving the other half to support normal function.
Despite the benefits, this technique isn’t suitable for all patients, said Dr Ng. Those who won’t be offered this option are those with large solid nodules (more than 3cm), making them difficult to remove through the 0.5cm incisions; those who are obese, making the surgical space too tight to work in; and those who require nasal intubation, as the nostrils may be injured during the procedure.
Although other surgical techniques developed in recent years are also able to avoid neck scars, they haven’t been popular with patients, with just 3 per cent of SGH patients opting for these methods.
More than 90 per cent continue to choose the conventional open method. Transaxillary and robotic thyroid surgeries involve incisions in the armpit, with the skin lifted off the muscles all the way to the neck for the camera and instruments to enter.
“Not all patients accept the idea of [surgery] going through the chest [in transaxillary surgery]. This is a sensitive area, and most patients are women,” said Dr Ng.
Robotic surgery, meanwhile, is substantially more expensive. These two methods also cause more bleeding and pain, as they involve a larger area of dissection.
The conventional method takes the shortest operating time – one to two hours – compared to as long as four for transaxillary and robotic, and two to three for transoral. Patients typically stay one to two days for all four methods.
SOURCE: SINGAPORE HEALTH. REPRODUCED WITH PERMISSION.
