The new Ward@Bowyer facility at Singapore General Hospital will start admitting confirmed and suspected Covid-19 patients from today. It will also admit patients with other infectious diseases, such as tuberculosis and measles. ST PHOTO: GAVIN FOO
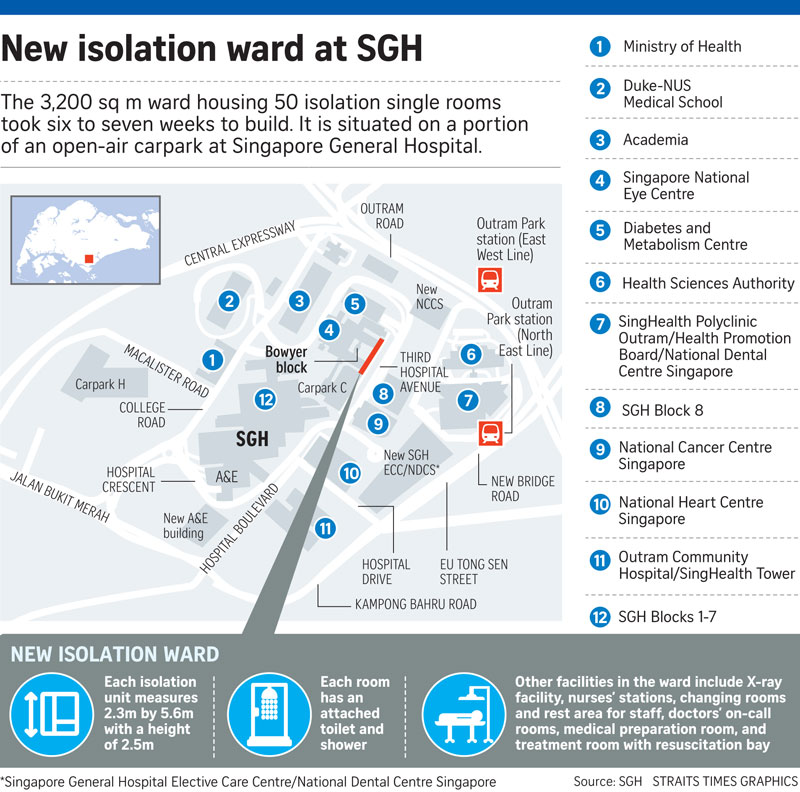
A new facility built on a portion of an open-air carpark in Singapore General Hospital (SGH) will add 50 isolation single rooms to the hospital's existing 35 to support the country's fight against Covid-19.
It will start admitting confirmed and suspected Covid-19 patients from today. The facility will also admit patients with other infectious diseases, such as tuberculosis and measles.
Work on the 3,200 sq m facility, which is named Ward@Bowyer as it is located adjacent to SGH's Bowyer Block, started in mid-May during the circuit breaker period and was completed over seven weeks.
The existing isolation ward for infectious diseases in SGH - Ward 68 - has 35 single rooms and 16 beds in non-single rooms.
Some of the roughly 300 Covid-19 patients in SGH during April and May had to be roomed in other wards, said the SGH medical board's chairman, Associate Professor Ruban Poopalalingam.
Of the 100 or so Covid-19 patients now in SGH, some - including incoming patients - will be sent to Ward@Bowyer.
The hospital sees 40 to 50 suspected Covid-19 patients each day.
The new ward is part of the national plan to increase capacity for Covid-19 cases, Prof Poopalalingam said. "This ward is not built as a permanent fixture for the long run. It is built to at least last the distance of the pandemic and hopefully beyond for other infectious diseases."
Ward@Bowyer is built to last a few years, he added.
"But we are happy with the increase in capacity of isolation rooms because (the ward) can be used beyond the Covid era. Apart from the National Centre for Infectious Diseases, there is not a lot of these infectious diseases isolation rooms in the country."
Patients who are sent to Ward@Bowyer must be able to walk about and take care of themselves, and have conditions assessed as less likely to deteriorate.
Each isolation room measures 2.3m by 5.6m with a height of 2.5m, and includes an attached toilet and shower. The rooms are designed to contain viral particles, which are then removed through specialised exhaust vents.
The medical team will use contact-free monitoring to detect warning signs of patient deterioration and will thus be able to intervene early.
For instance, patients will be given a biosensor to wear on their wrists which will allow their heart rate, respiration rate and oxygen saturation level readings to be wirelessly transmitted to clinicians.
 The patients can also check their own vital signs as the information will be sent to a mobile app which they can access through in-room smartphones.
The patients can also check their own vital signs as the information will be sent to a mobile app which they can access through in-room smartphones.
If the patients are unwell or need assistance, they can use the in-room smartphone to contact the medical team either through videoconferencing or an app called MyCare Lite, which was developed by SGH's Nursing Division and the Integrated Health Information Systems, the Ministry of Health's IT arm.
By leveraging technology, the medical team can efficiently monitor and interact with patients without unnecessary risk of exposure, said SGH.
The smartphone also contains pre-loaded games to help patients pass the time, as well as reading materials about Covid-19 and coping with isolation.
Each isolated patient, who needs to wear a mask at all times, will be given an admission pack containing surgical masks, a digital thermometer and toiletries, and a care pack filled with drinks and snacks.
