Vascular anomalies are a heterogeneous group of conditions that involve abnormal growth or arrangement of various forms of blood or lymphatic vessels in the body. According to the International Society for the Study of Vascular Anomalies (ISSVA), vascular anomalies can be classified into two broad categories – vascular tumours and vascular malformations (Figure 1).
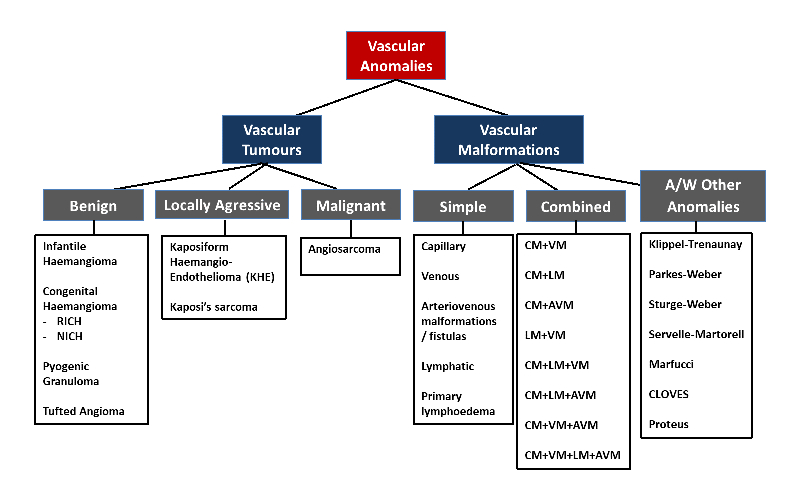
Figure 1. ISSVA Classification of Vascular Anomalies 2018 (abridged)
Vascular tumours and malformations range from mild to severe conditions that can lead to significant physical, psychological and emotional impairment. Small infantile haemangiomas or capillary malformations, especially those not on critical sites (e.g. arms, legs and trunk) can be followed in the primary care setting. More complex and severe vascular anomalies should ideally be managed under the care of a multidisciplinary team in centres specialising in the management of complex vascular anomalies. A combination of various treatments involving input from various subspecialties may be required for optimal results.
Diagnosis and treatment
The ISSVA classification of vascular anomalies has led to standardisation of the nomenclature. This is important as there now exists a variety of treatment options targeted at the various vascular tumours and malformations. Accurate diagnosis is key to inform appropriate treatments and optimal outcomes.
Typical treatment modalities include systemic medications, interventional radiological procedures (e.g. sclerotherapy and embolisation), surgery, lasers and physical therapy. Timely and effective multidisciplinary treatment can result in good results in many patients (Figure 2).
 |  |
|
Figure 2. Patient with ulcerate infantile haemangioma before and after multi-modality treatment with oral propranolol, oral prednisolone, wound dressings and pulsed dye laser therapy. |
Specific treatments targeting mutations in gene pathways are developing more recently, paving the way for more targeted treatments with improved efficacy. Germline and somatic mutations involving the
PIK3CA or
RAS-RAF-MEK-ERK gene pathways have been identified in many vascular anomalies.
mTOR (Mammalian Target Of Rapamycin) inhibitors such as sirolimus and everolimus exert anti-proliferative properties. They have shown efficacy in the treatment of various vascular anomalies, including vascular tumours such as kaposiform haemangioendothelioma and vascular malformations such as lymphatic malformations and venous malformations.
More specific
PIK3CA inhibitors (e.g. alpelisib) are now being evaluated for the treatment of complex vascular anomalies, as are
MEK inhibitors (e.g. trametinib).
Multidisciplinary management for vascular anomalies
The treatment of complex vascular anomalies requires a multidisciplinary and multi-modality approach, often involving input from various subspecialties. The
multidisciplinary vascular anomalies team at KK Women’s and Children’s Hospital (KKH) comprises experts in the fields of dermatology, interventional radiology, paediatric haematology/oncology, plastic surgery, paediatric surgery and orthopaedic surgery.
Other subspecialties that contribute to the diagnosis and management of patients with vascular anomalies include genetics, paediatric gastroenterology, respirology, ophthalmology, otolaryngology, physiotherapy, occupational therapy, speech and language therapy, and psychology.
Together with the multidisciplinary vascular anomalies team at Singapore General Hospital (SGH), both KKH and SGH are members of the SingHealth Duke-NUS Vascular Centre, enabling a one-stop centre for the diagnosis and management of a wide range of vascular anomalies in children, adolescents (seen at KKH) and adults (seen at SGH).
Case study: Treating a young woman with extensive venous malformation M presented to the Vascular Anomalies Clinic at KKH with extensive venous malformation of her lip, tongue and buccal mucosa (Figure 3A). These were present at birth and had gradually increased in size over the years. Imaging revealed deeper involvement including the pharynx and larynx, with narrowing of her upper airways. While M had previously sought advice from other healthcare providers, no single treatment had been deemed to be effective and safe due to the extent of airway involvement. With discussion amongst the multidisciplinary vascular anomalies team at KKH, a targeted and holistic management plan was put in place for M. This involved multi-modality treatment with oral sirolimus, multiple treatment sessions for sclerotherapy, and pulsed dye laser and Nd-YAG laser treatment over two to three years. M was continually reviewed by the multidisciplinary care team at KKH, and her care was subsequently transitioned to the team at SGH. Post-treatment, there was marked improvement in the size of the venous malformation, both externally and internally (Figure 3B), which has enabled her speech to become clearer. M and her family were happy with the results and she is now a more confident young woman. M continues to be reviewed by her multidisciplinary care team. |
 |
 |
|
Key points: - Complicated vascular anomalies should be managed by a multidisciplinary team.
- A majority of vascular anomalies can be diagnosed through history, clinical examination and confirmed on imaging. In atypical cases, histology may be necessary.
- Infantile haemangiomas are the most common vascular tumours in children. Complex cases can be treated successfully with topical or systemic beta-blockers.
- Vascular malformations can present at birth or later in childhood, and most do not undergo spontaneous resolution.
|
 |
Associate Professor Mark Koh, Head and Senior Consultant, Dermatology Service, KK Women’s and Children’s Hospital Assoc Prof Mark Koh is a dermatologist who specialises in paediatric dermatology and dermatopathology. Assoc Prof Koh also a visiting consultant at Singapore General Hospital (SGH), Sengkang General Hospital and National Cancer Centre Singapore. Assoc Prof Koh is Clinical Associate Professor, Duke-NUS Medical School; Adjunct Associate Professor, Lee Kong Chian School of Medicine, Nanyang Technological University (NTU); and Senior Clinical Lecturer, Yong Loo Lin School of Medicine, National University of Singapore (NUS). |
 |
Dr Luke Toh, Head and Senior Consultant, Interventional Services, Department of Diagnostic and Interventional Imaging, KK Women’s and Children’s Hospital Dr Luke Toh had received his fellowship training in paediatric interventional radiology, and is a diagnostic radiologist with special interest in the management of vascular malformations. Dr Toh is also Deputy Head, Department of Diagnostic and Interventional Imaging, KKH, and a visiting consultant at the Department of Vascular and Interventional Radiology at SGH. Dr Toh is Clinical Assistant Professor, Duke-NUS Medical School; and Adjunct Assistant Professor, Department of Anatomy, Yong Loo Lin School of Medicine, NUS. |
 |
Associate Professor Chan Mei Yoke, Senior Consultant, Haematology/Oncology Service, KK Women’s and Children’s Hospital Assoc Prof Chan Mei Yoke is a paediatric haematologist/oncologist and palliative care specialist. Assoc Prof Chan trained at the Vascular Anomalies Center at Boston Children’s Hospital, USA and contributed to the development of the multidisciplinary Vascular Anomalies Clinic at KKH to manage complex vascular anomalies. Assoc Prof Chan is a Clinical Associate Professor with Duke-NUS Medical School, NUS Yong Loo Lin School of Medicine and NTU Lee Kong Chian School of Medicine. |
References: - ISSVA classification for vascular anomalies (2018). Retrieved from
https://www.issva.org/UserFiles/file/ISSVA-Classification-2018.pdf
- Harter N, Mancini AJ. Diagnosis and management of infantile hemangiomas in the neonate. Pediatr Clin North Am 2019;66:437-459
- Hammill AM, et al. Sirolimus for the treatment of complicated vascular anomalies in children. Pediatr Blood Cancer 2011;57:1018-1024
- Zuniga-Castillo M, Teng CL, Teng JMC. Genetics of vascular malformation and therapeutic implications. Curr Opin Pediatr 2019;31:498-508
- Martinez-Lopez A, et al. Vascular malformations syndromes: an update. Curr Opin Pediatr 2019; Jul 29. doi: 10.1097/MOP.0000000000000812. (Epub ahead of print)
|

