Stroke is an enormous public health problem worldwide. National Heart Centre Singapore shares on hyper-acute stroke treatment.
Stroke is an enormous public health problem worldwide. The National Registry of Diseases Office reported that in 2014, there were about 7000 cases in Singapore, which approximates 20 cases per day. Most of those affected are aged over 60, and about 80% are ischaemic strokes. Stroke also ranks consistently amongst the top 5 causes of death in our country.
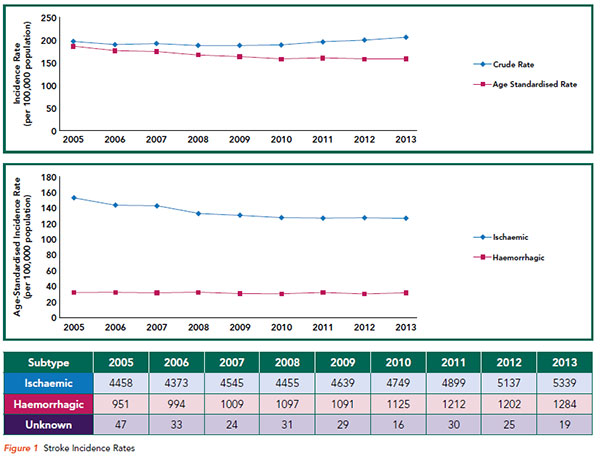
With better understanding of Pathophysiology and primary prevention, the age-specific incidence of stroke in Singapore has been declining. However, the absolute number of patients each year has been gradually increasing, likely due to demographic shifts. (Refer to Figure 1)
WHAT HAPPENS AFTER A STROKE?
Results from the Oxfordshire Community Stroke Project showed1 that, at 1 year after a stroke, approximately 23% of patients have demised. Amongst the survivors, about 35% are dependent in their activities of daily living (ADLs). In practice, the potential for permanent disability with a severely compromised quality of life is often the greatest fear patients have, sometimes even exceeding the fear of death itself.
The socio-economic burden is also significant, as stroke is a leading cause of adult disability in developed countries.
CAN WE PREVENT DISABILITY IN STROKE PATIENTS?
Animal studies in the 1980s by Astrup et al2 showed that following acute vascular occlusion, not all brain tissue within an arterial territory infarcts immediately. Within the area of Oligaemia, there is a “penumbra”, where the neuronal tissue, though non-functioning, remains viable. If perfusion could be restored quickly, these neurons could be salvaged and their function restored. It was theorised that stroke patients benefit similarly from penumbral salvage.
This hypothesis was proven in 1995, in the NINDS trial of tissue plasminogen activator for acute ischaemic stroke3. In this randomised controlled trial, 622 patients presenting within 3 hours of stroke onset were randomised to receive either Intravenous (IV) Alteplase at 0.9mg/kg or placebo.
At 3 months post-stroke, significantly more patients in the Alteplase group (39%) were able to return to all their previous activities (mRS 0 - 1) as compared to the placebo group (26%). This was not without risk, as the risk of symptomatic intracranial haemorrhage was at 6.6% in the Alteplase group, versus 0.6% in the placebo group. However, overall, mortality was similar in both groups at 3 months poststroke. (Refer to Figure 2)
The time window for IV Alteplase was later extended from 3 hours to 4.5 hours with the conclusion of the European ECASS III trial in 20084; though predictably, the observed benefit was less, when compared to the original NINDS trial. The Number Needed to Treat (NNT) for a functional outcome of mRS 0 - 1 at 3 months post-stroke rose from 8 to 14.
|
Modified Rankin Scale (mRS) | Description |
| 0 | No symptoms. |
| 1 | No significant disability. Able to carry out all usual activities, despite some symptoms. |
| 2 | Slight disability. Able to look after own affairs without assistance, but unable to carry out all previous activities. |
| 3 | Moderate disability. Requires some help, but able to walk unassisted. |
| 4 | Moderately-severe disability. Unable to attend to own bodily needs without assistance, and unable to walk unassisted. |
| 5 | Severe disability. Requires constant nursing care and attention, bedridden, incontinent. |
| 6 | Death |
Figure 2 Modified Rankin Scale (mRS)
ENDOVASCULAR CLOT RETRIEVAL
The next significant breakthrough in hyper-acute stroke treatment came in 2015. Intravenous (IV) Thrombolysis was considered the standard of care at this stage. However, patients with occlusions of the large arteries in the anterior circulation still did poorly, as these tended not to recanalise with Alteplase alone; in fact, early recanalisation occurred in approximately 1/3 of patients with internal carotid artery occlusions.
The Dutch investigators in the MR CLEAN trial5 randomised 500 patients into 2 arms, one receiving endovascular treatment plus usual care (which may include IV Thrombolysis), and the other receiving only usual care (IV Alteplase within 4.5 hours of onset, if no contraindications were present). Patients presenting with a radiographically proven occlusion of the Internal Carotid Artery (ICA), or the first 2 segments of the Middle Cerebral Artery (MCA) or Anterior Cerebral Artery (ACA), and who were able to receive endovascular treatment within 6 hours of stroke onset, were recruited.
At 3 months post-stroke, patients who received endovascular treatment were 2 times more likely to achieve an mRS of 0 - 2 (32.6% versus 19.1% or 2.16%). Following this, 5 other RCTs reporting positive results for endovascular treatment were published6–10, albeit each with slightly different selection criteria and treatment protocols, but overall, displaying the powerful treatment effect of EVTs (Endovascular Thrombectomy) 11. (Refer to Figure 3)

ENDOVASCULAR THROMBECTOMY (EVT) WITHOUT THROMOBOLYSIS
What was not very clear at the time was whether Endovascular Thrombectomy (EVT) alone would be effective for treating these patients, as there were only small numbers of them in the aforementioned RCTs.
I was on HMDP fellowship then, and the hospital I was in, was 1 of 2 tertiary centres providing neurointerventional services to the state of Western Australia. Many patients were arriving within the time frame for EVT, but were out of the 4.5-hour window period for IV Thrombolysis.
Yet others came within the 4.5-hour window period, but had clear contraindications to Alteplase, such as having undergone recent surgeries. With this in mind, we initiated a retrospective registry, based on the study of acute stroke cases who had received EVT12.
Between the period of October 2013 to April 2016, there were 50 patients, with strokes secondary to a proximal occlusion in the anterior cerebral circulation, that received EVT. Contrary to the RCTs where only 15% of patients did not receive Alteplase, we found that in the real-world application, 58% of patients were ineligible for Alteplase.
Outcomes using the surrogate of the National Institute of Health Stroke Scale (NIHSS) showed an improvement of 8 points at 24 hours or a NIHSS of 0 – 2, which was similar between the 2 groups. These findings added to the body of literature that was being published concurrently, supporting the use of EVT in Alteplase-ineligible patients.
CURRENT MANAGEMENT OF STROKE PATIENTS: SGH AND NNI-PARTNER HOSPITALS
Keeping in mind that time is critical for the acute management of stroke patients, we engaged our partners in Civil Defence, who responded enthusiastically.
Ambulance paramedics are now trained in the use of the Cincinnati Prehospital Stroke Scale to make a preliminary diagnosis of an acute stroke. Emergency departments are pre-notified and patients are given priority access to neurologists and CT/MRI scans.
Once a diagnosis of an acute ischaemic stroke is established, eligible patients are given IV Alteplase within 4.5 hours, with 10% of the dosage as a bolus and the remainder as an infusion over the course of an hour. For patients with a suspected occlusion of the proximal anterior circulation within 6 hours of onset, a CT/ MR angiography is typical.
If a clot is found, the neurointerventionalist is informed and a decision is made regarding EVT. This is performed on-site at the Singapore General Hospital and the Tan Tock Seng Hospital. A “drip and ship” model is employed in other hospitals covered by NNI neurologists, where Intravenous Alteplase is initiated and the infusion is given en route to the patient, whilst being transferred to an end-vascular facility.
“TIME IS BRAIN”
Regardless of whichever hospital the stroke patient initially arrived in, the key is timely intervention. It was estimated that for strokes due to a large vessel occlusion, 1.9 million neurons are lost each minute.
Many patients are still unaware of the necessary urgency of stroke treatment and seek emergency assistance for acute treatment beyond the required time frame. Some patients even arrive days after the onset of stroke. Despite the many treatment advances in recent years, little is available to help them.
WHAT CAN GENERAL PRACTITIONERS DO?
As primary care partners, we hope that you can help to educate patients on the symptoms of stroke and the need for emergency care. In particular, this includes elderly patients and those with cardiovascular risk factors.
Should a patient visit the clinic with an acute stroke, it is probably better to send them for treatment via the emergency ambulance (in view of the priority access given), rather than through other forms of transport.
GPs can call for appointments through the GP Appointment Hotline at 6357 7095 or scan the QR code for more information.
By: Dr Wee Chee Keong, Consultant, Department of Neurology, National Neuroscience Institute (NNI)
Dr Wee Chee Keong is a Neurologist at the
National Neuroscience Institute (NNI). He has a keen interest in ischaemic strokes and reperfusion therapies. He recently returned from a year-long fellowship with Professor Graeme J. Hankey at Sir Charles Gairdner Hospital in Perth, with a focus on hyper-acute stroke treatment.
Back in Singapore, he contributes actively to the acute stroke team, members of whom are rostered every day of the year to help provide treatment to the stroke patients at the hospital.
References
1. Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project--1981-86. 2. Incidence, case fatality rates and overall outcome at one year of cerebral infarction, primary intracerebral and subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry 1990;53(1):16–22.
2. Astrup J, Siesjö BK, Symon L. Thresholds in cerebral ischaemic - the ischaemic penumbra. Stroke J Cereb Circ 1981;12(6):723–5.
3. Tissue plasminogen activator for acute ischaemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333(24):1581–7.
4. Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischaemic stroke. N Engl J Med 2008;359(13):1317– 29.
5. Berkhemer OA, Fransen PSS, Beumer D, et al. A Randomized Trial of Intraarterial Treatment for Acute Ischaemic Stroke. N Engl J Med 2015;372(1):11–20.
6. Goyal M, Demchuk AM, Menon BK, et al. Randomized Assessment of Rapid Endovascular Treatment of Ischaemic Stroke. N Engl J Med 2015;372(11):1019–30.
7. Campbell BCV, Mitchell PJ, Kleinig TJ, et al. Endovascular Therapy for Ischaemic Stroke with Perfusion-Imaging Selection. N Engl J Med 2015;372(11):1009–18.
8. Saver JL, Goyal M, Bonafe A, et al. Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. N Engl J Med 2015;372(24):2285–95.
9. Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 Hours after Symptom Onset in Ischaemic Stroke. N Engl J Med 2015;372(24):2296–306.
10. Bracard S, Ducrocq X, Mas JL, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 2016;15(11):1138–47.
11. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. The Lancet 2016;387(10029):1723–31.
12. Wee C-K, McAuliffe W, Phatouros CC, et al. Outcomes of Endovascular Thrombectomy with and without Thrombolysis for Acute Large Artery Ischaemic Stroke at a Tertiary Stroke Centre. Cerebrovasc Dis Extra 2017;7(2):95–102.
