The clinical presentation of a young infant often crying for long hours and mostly in the evening, for reasons that may not be immediately apparent, is a common situation experienced by many primary healthcare providers.
Infantile colic, diagnosed according to the Rome IV criteria, is the clinical presentation of an infant who has cried or fussed for three or more hours a day, during three or more days in the preceding week – with the history confirmed by a 24-hour behaviour journal maintained by the caregiver1. The caregiver will need to record the duration and frequency of crying, the infant’s feeding pattern, bowel output and any other associated symptoms.
This behavioural phenomenon often presents in the first month of life, and continues until four to six months of age. While managing a crying infant can be a distressing routine for caregivers, fortunately this behaviour generally starts to improve by the time weaning is introduced.
Determining the right cause
The true incidence and prevalence of infantile colic can be challenging to estimate, as its aetiology is complex and ill-defined, and symptoms can be vague and non-specific. Further, varying diagnostic criteria are applied in different parts of the world, and parental perception of fussiness or abnormal crying can be subjective, influencing the eventual diagnosis.
The clinical phenomenon is thought to be caused by various factors which include altered gut motility, gastro-oesophageal reflux, milk protein allergy or intolerance, lactose intolerance or intestinal distension from increased bowel gas and altered intestinal microbiome2, 3.
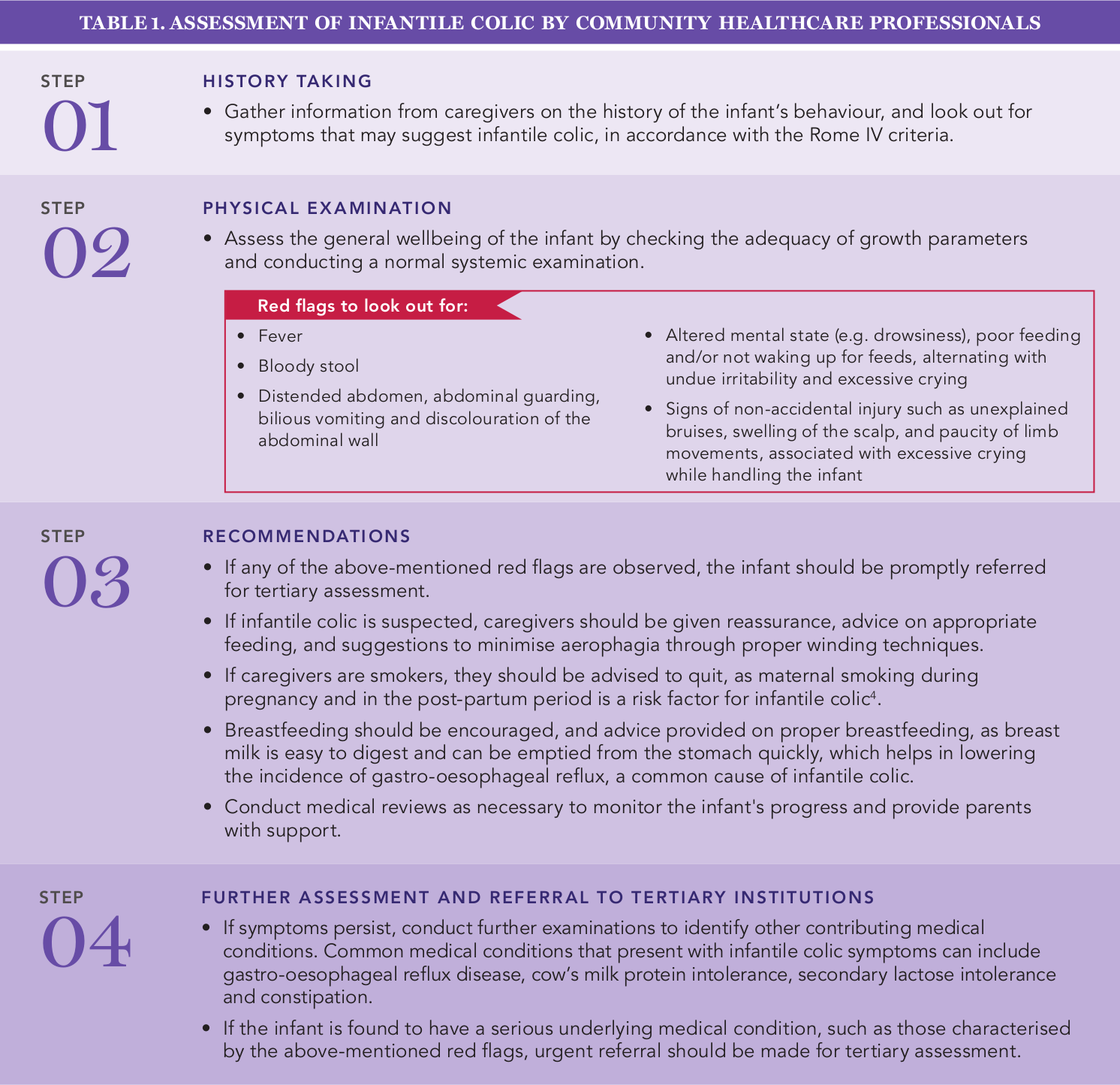
In a small number of infants, this behaviour may be associated with more serious medical conditions such as intussusception, visceral pain, cerebral irritation from infections, or non-accidental injuries. In such cases, nonspecific and excessive crying may be the only presenting symptom. The steps for assessment of infantile colic by community healthcare practitioners are outlined in Table 1.
Treatment and intervention
In the absence of pathological concerns, infantile colic is self-limiting and has a good prognosis. In these instances, the condition can be effectively managed by providing caregivers with management advice, caring reassurance and regular follow-up for the infant.
While some caregivers may opt for over-the counter formulations to soothe their crying babies, there is currently no strong scientific evidence to recommend their routine use in clinical practice.
The majority of young infants who present to the General Paediatrics Service at KK Women’s and Children’s Hospital with non-specific and excessive crying do not have serious medical problems. However, should a potential underlying medical condition be identified, timely and appropriate referral for tertiary assessment and intervention is beneficial in managing the infant’s condition, and minimising the distress experienced by both caregiver and child.
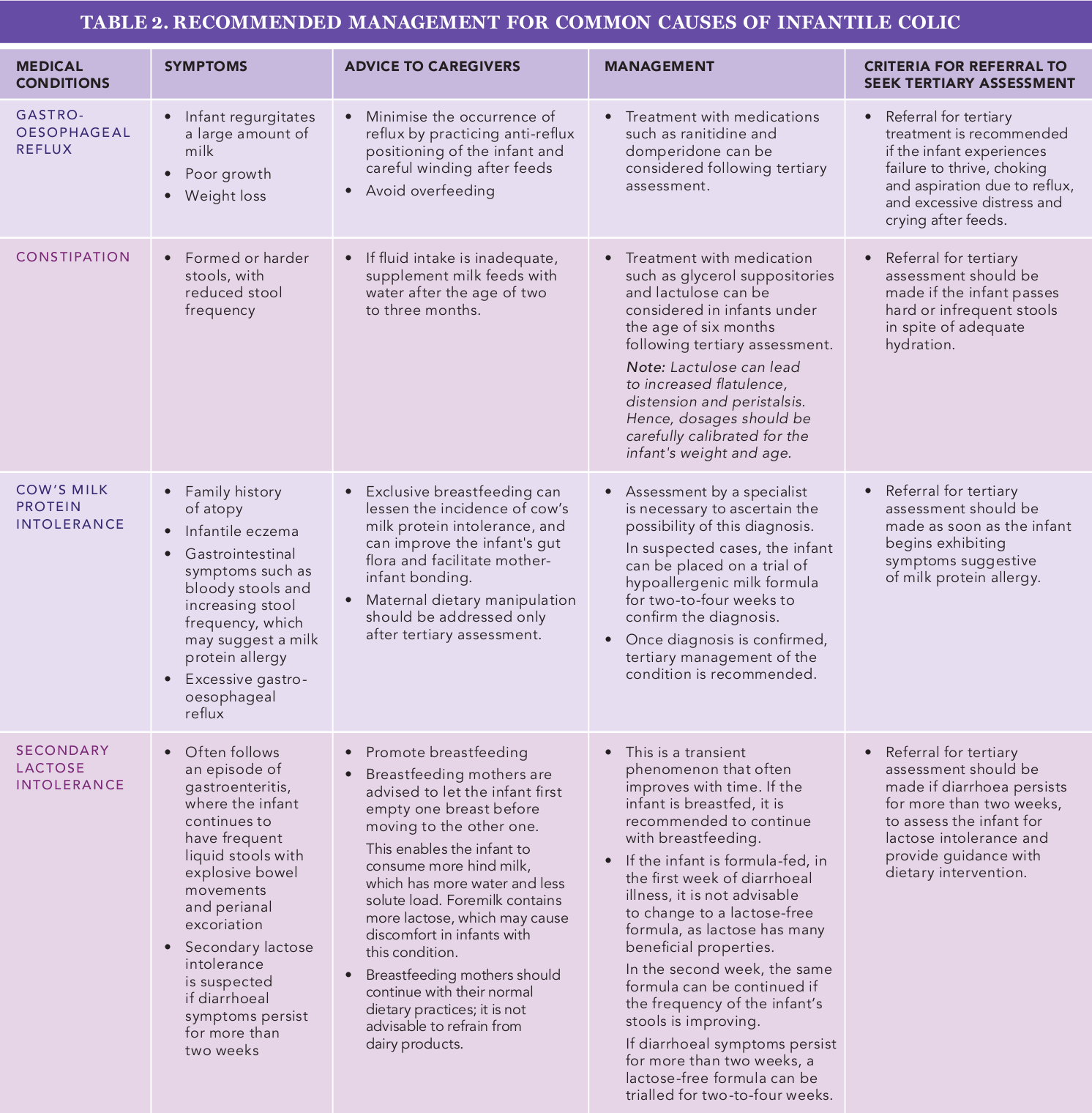
Table 2 outlines some common causes of infantile colic, their management recommendations and criteria for tertiary assessment.
Refer a patient
Polyclinics and community healthcare practitioners can contact KKH at
+65 6294 4050 to refer patients to the General Paediatrics Service for tertiary assessment and management for infantile colic. |
References: - Judith Zeevenhooven, Ilan J.N. Koppen, and Marc A. Benninga. The New Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers. Paediatric Gastroenterology, Hepatology & Nutrition 2017 March 20(1):1-13
- Hill, David J.; Hosking, Clifford S. Infantile Colic and Food Hypersensitivity. Journal of Paediatric Gastroenterology and Nutrition 2000; 30(1): pp S67-S76
- Heine, Ralf G. Gastroesophageal refl ux disease, colic and constipation in infants with food allergy Current Opinion in Allergy and Clinical Immunology 2006; 6:220-225
- Charlotte Søndergaard; Tine Brink Henriksen; Carsten Obel; and Kirsten Wisborg. Smoking during Pregnancy and Infantile colic. Pediatrics 2001; 108:342-346
|

