A mammogram is an X-ray examination of the breast, and is often used as a screening tool to check for
breast cancer in women who have no signs or symptoms of the disease. A
mammogram can also be used as a diagnostic and interventional imaging tool in women experiencing symptoms suggestive of breast cancer, such as a lump, pain, skin dimpling or nipple discharge.
To date, mammography is the only screening modality shown to reduce breast cancer mortality. However, full field digital mammography is a two-dimensional modality in which overlapping breast tissues can pose diagnostic difficulty resulting in false negative and false positive findings. In breasts with dense tissues, the sensitivity of mammography can decrease by up to 50 percent.
Introduced in KK Women’s and Children’s Hospital (KKH) in 2015 and a first for restructured hospitals in Singapore, CESM technology combines the benefits of both full field digital mammography and intravenous contrast media utilisation, providing valuable information to guide the assessment and management of breast abnormalities, cancer and indeterminate findings on mammography and/or ultrasound.
Other advantages of this relatively new modality include high diagnostic accuracy, cost-effectiveness, shorter waiting time to definitive treatment and the ease of image acquisition. As the use of CESM techniques continues to evolve, its use looks set to further improve patient care and experience, particularly in the area of breast cancer diagnosis and treatment.
Contrast enhnaced visualisation
CESM is performed after administration of intravenous iodinated contrast medium. Utilising the concept of new blood vessel formation observed in tumours, the injected contrast agent highlights areas of blood vessel proliferation within tumours, making them more visible on mammogram.
The dual energy CESM technique takes advantage of the differences in X-ray attenuation between iodinated contrast material and breast tissue to further enhance the visualisation of tumours within the breast.
During the examination process
At KKH, mammography is carried out by female radiographers. The iodinated contrast medium is administered into the patient through an intravenous cannula, and two sequential images of both breasts are taken at low and high energies.
The low energy image is similar to a standard full field digital mammography image, which provides soft tissue and calcification detail. The high energy image demonstrates the iodine contrast enhanced areas. These two images are digitally subtracted from one another to produce an image that highlights areas of contrast enhancement.
Indications for CESM
Established indications for screening with CESM include criteria indicating the patient is at high risk for breast cancer. This includes at least one of the following:
- Known BRCA1 and BRCA2 mutations
- Family history of both breast and ovarian cancer
- two or more first degree relatives with breast or ovarian cancer
- Breast cancer occurring before the age of 50 years in a close relative
Case study: Evaluating a patient for breast cancer in the contralateral breast
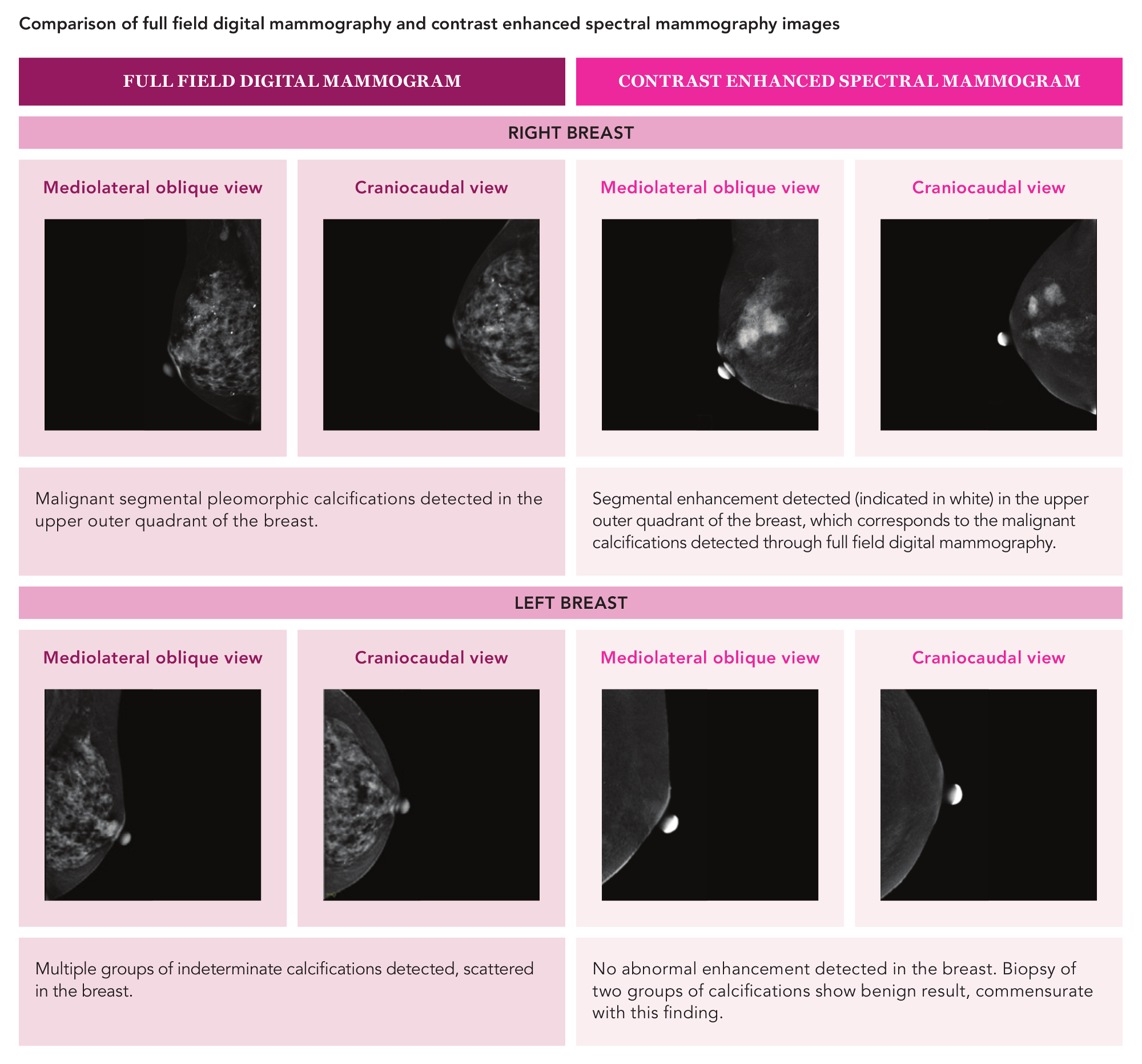
Hui (not her real name), a 65-year-old Chinese lady presented with a hard lump in her right breast. Her late mother had been diagnosed with breast cancer at the age of 33 years and died in the same year. A full field digital mammogram showed widespread suspicious calcifications in the upper right breast, and multiple clusters of moderately suspicious calcifications scattered in the left breast. Ultrasound of the upper right breast confirmed the presence of a suspicious solid mass, which was biopsied under ultrasound guidance and a diagnosis of cancer was confirmed. As cancer had been diagnosed in the right breast, the clinical question was - were there additional foci of cancer in the left breast? Which cluster of calcifications out of the many clusters of calcifications should be evaluated, taking into consideration the patient’s ability to tolerate biopsy of multiple areas within the breast? To further enhance the visualisation of calcifications and tumours within both breasts, CESM was performed. The proven cancer in the right breast showed abnormal enhancement, the size of which correlated well with the tumour size depicted on mammography and ultrasound. Further, the histopathological size of the cancer in the mastectomy specimen correlated with the size of the enhancement seen on CESM. In the left breast, no abnormal enhancement was seen. Two clusters of calcifications which were deemed most suspicious were subsequently biopsied; both showed benign result consistent with the negative CESM result. The likelihood of cancer in the breast with a negative CESM result is very low. This case illustrates the value of CESM in providing clarity and conclusiveness to the assessment of tumour size and evaluation of the contralateral breast for additional foci of cancer. Through the use of CESM, invasive procedures and biopsies of certain lesions in patients diagnosed with breast cancer can be averted. |
A compelling alternative to MRI
CESM is a useful tool in cancer staging and can serve as a compelling alternative to patients requiring magnetic resonance imaging (MRI) of breasts for further work up. This can be especially valuable for patients with contraindications to MRI such as the presence of a pacemaker, allergy to a contrast agent or severe claustrophobia.
Further, studies have shown that CESM is comparable to MRI for the depiction of the index tumour. While CESM is less sensitive than MRI in the detection of additional sites of cancer, the added sensitivity of MRI has to be weighed against the higher frequency of false positive results.
These false positive results can lead to the increased need for biopsies and mastectomies, which may delay the time to definitive treatment. In comparison to MRI, breast examination by CESM is more cost-effective for patients.
It is also time-saving, as the preparation and process of an examination is typically 30 to 45 minutes. MRI preparation and process typically requires about 75 minutes to complete.
CESM is also useful in the assessment of inconclusive findings that cannot be clarified by conventional mammography and/or ultrasound. CESM, like MRI, can be used in inconclusive findings because the possibility of cancer is virtually ruled out if the examination is negative.
For patients with dense breast tissue, within which cancer lesions can often be obscured, CESM can be useful in detecting additional cancerous lesions within the same breast or contralateral breast.
For patients with multiple solid nodules within the breasts, CESM can help the radiologist to determine which nodules may require biopsy based on the enhancement pattern. CESM can also be used to monitor the patient’s response to neoadjuvant chemotherapy, especially in patients with contraindications to MRI.
An evolving technology
With CESM, the assessment of very posteriorly located lesions may be limited, specifically chest wall invasion and evaluation of internal mammary lymphadenopathy. Additionally, technology to target areas of abnormal enhancement for tissue diagnosis using CESM is currently unavailable.
However, the development of CESM-guided biopsy technique is underway. Until CESM-guided biopsy becomes available, second look ultrasound is used to find a sonographic correlate for abnormal areas of enhancement so tissue sampling can be obtained under ultrasound guidance.
False negative results may be seen with small cancers or low grade histology due to minimal enhancement. False positive results may be seen in enhancement of benign lesions.

