Coronary artery bypass grafting (CABG) is a surgical procedure in which patient’s own blood vessels are used as graft to bypass narrowed or blocked coronary arteries.
Coronary artery bypass grafting (CABG) is a surgical procedure in which patient’s own blood vessels are used as graft to bypass narrowed or blocked coronary arteries. It helps improve blood and oxygen supply to the heart and thus improve patients’ symptoms and enhance quality of life.
By Dr Tham Yi Chuan, Associate Consultant, Department of Cardiothoracic Surgery
The development of coronary angiogram in the 1960s, allowed the identification of diseased coronary artery, and hence laid down the foundation in understanding and treatment of this disease. While many sporadic efforts were made to treat this
disease, we cannot run away from discussing CABG without first mentioning Vineberg and Favaloro.
Arthur M. Vineberg, the immediate forerunner of CABG1, developed the procedure of direct implantation of internal mammary artery into myocardium in 1951, with the operation later known as ‘the Vineberg operation’. It received widespread clinical application during the 1960s and decades later, it was demonstrated that this procedure brought new blood flow to the left ventricular myocardium. Then in 1967, Rene Favaloro, the pioneer and ‘father’ of CABG, began performing CABG with vein graft, hence creating blueprint of how CABG is performed today.
The CABG Surgery
CABG is a type of revascularisation procedure used to treat coronary artery heart disease and restore or increase blood supply to the myocardium (muscles of the heart). Patients with coronary artery disease may face risk of angina (chest pain caused by reduced blood flow to the heart), and if severe, may require CABG to improve blood supply. For these patients, there is also a risk of getting heart attack.
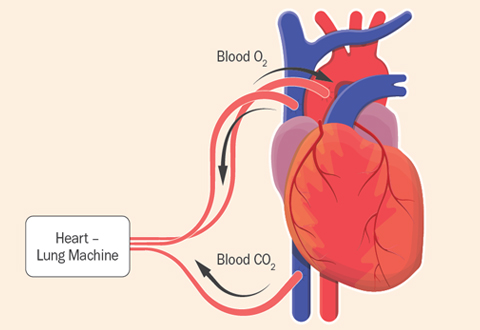
The heart and lung bypass machine does the work of the heart and takes over the pumping of the blood when the heart is stopped.
Long-term Benefits & Latest Developments
The evidence of CABG is undisputable, with the disease being one of the most researched topics in the history of medicine. From the pivotal randomised controlled trial in the 1970s and 80s (Veteran Administration Cooperative Study, European Coronary Surgery Study and Coronary Artery Surgery Study), they had cemented CABG as one of the most important treatments for patient with coronary artery disease. The relative survival benefit of CABG over medical therapy is consistent across many studies. However, because of the early surgical risk associated with CABG, its survival advantage does not become apparent until one to two years after surgery and they tend to increase with longer follow-up.
SYNTAX trial is another landmark study that compared CABG to PCI2. Overall, patients with three-vessel disease (TVD) in this study had survival benefit with CABG, and in particular, patients with more complex TVD undergoing CABG had better long-term outcome compared to patients that had PCI. Patients with diabetes mellitus especially, have improved outcome when undergoing CABG compared to PCI, with less patients had to return for repeat revascularisation procedure.
Many attempts have been made to improve outcomes of CABG. Minimally-invasive CABG seeks to reduce the invasiveness of the conventional sternal-splitting CABG. Additionally, CABG could be performed without heart-lung machine. Recently, there is also growing interest in hybrid revascularisation procedure, however, with different measurement outcomes. Despite the various attempts, the only time-tested outcome improving technique in recent years is to increase the number of arterial grafts when performing CABG.
Key to Best Outcomes
Many patients thought that CABG cures coronary artery disease. In fact, CABG only address the consequences of underlying multiple cardiac risk factors that contributed to development of the disease, it does not prevent the progression of disease. CABG is a matured procedure in the treatment of coronary artery disease and it is very effective in providing durable relief of angina and performed primarily to improve survival of patients with coronary artery disease. The essence of good treatment lies with the joint decision-making process of patients and their cardiac surgeons and cardiologists. Guideline-directed medical therapy that includes adoption of lifestyle modification are the key to improved long-term outcomes.
In conclusion, CABG has proven to provide significant improvement in symptoms, quality of life and survival for appropriately selected patients with multi-vessel coronary artery disease. Patients with more advanced multi-vessel coronary artery disease, left ventricular dysfunction or diabetes are particularly likely to benefit from CABG.
1 The Vineberg procedure: the immediate forerunner of coronary artery bypass. J B Shrager. Ann Thorac Surg. 1994 May
2 PW Serruys et al. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N Engl J Med 2009; 360:961-972
General references:
JH Alexander and PK Smith. Coronary-Artery Bypass Grafting. N Engl J Med 2016; 374:1954-64
4th Edition Kirklin Barratt-Boyes Cardiac Surgery textbook
This
article is from Murmurs Issue 43 (May – August 2022). Click here to read other articles or issues.
