Citrin deficiency is an autosomal recessive inborn error of metabolism (IEM) which can manifest in three distinct age-dependent clinical phenotypes. In the neonatal age group, it can present as neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD), characterised by prolonged cholestatic jaundice and possible liver dysfunction. In childhood, it can present as failure to thrive and dyslipidemia caused by citrin deficiency (FTTDCD), characterised by poor weight gain. In adulthood, citrin deficiency can present as citrullinemia type 2, characterised by neurologic and psychiatric symptoms.
As a normal newborn metabolic screening result does not exclude the diagnosis of NICCD, it is crucial for healthcare providers to maintain a high level of suspicion for infants presenting with prolonged (i.e. more than 14 days for full term infants and more than 21 days for preterm infants) conjugated jaundice, infantile cholestasis and positive urinary reducing substance (URS) tests. Additionally, a small percentage of infants with NICCD will develop citrullinemia type 2; hence ongoing health surveillance into adulthood is essential.
What causes citrin deficiency?
Citrin deficiency is associated with mutations in the
SLC25A13 gene. Mutation in
SLC25A13 affects the function of aspartate/glutamate carrier 2 (AGC2) in the inner mitochondrial membrane. AGC2 transports aspartate into the cytosol, which is then used to generate arginosuccinic acid in the urea cycle. Aspartate in the cytosol also helps with the oxidation of nicotinamide adenine dinucleotide and hydrogen (NADH), and subsequently NADH-reduced equivalents can be transported into the mitochondrial matrix for adenosine triphosphate (ATP) synthesis by the respiratory chain complex.
When AGC2 is not working well, the urea cycle is disrupted. It can also cause NADH to accumulate in the cytosol which may result in energy shortage in the cell, especially in hepatocytes, where AGC2 is highly expressed. NADH build-up also inhibits the metabolism of galactose, a simple sugar, due to impairment of the uridine diphosphate galactose 4’-epimerase enzyme, resulting in elevated levels of galactose in the urine (galactosuria) and blood (galactosemia).
In the western population, classic galactosemia in infants is often associated with reduced levels of gal-1-phospahate-uridyltransferase (GALT) enzyme activity. However, in East-Asian races, the prevalence of classic galactosemia is very low, whilst galactosemia due to NICCD is more common, as NICCD has a high prevalence in Asia. The carrier frequency for citrin deficiency in China is reported to be one in 65 while the carrier frequency in Singapore is reported to be one in 41.
Screening and diagnosis for NICCD
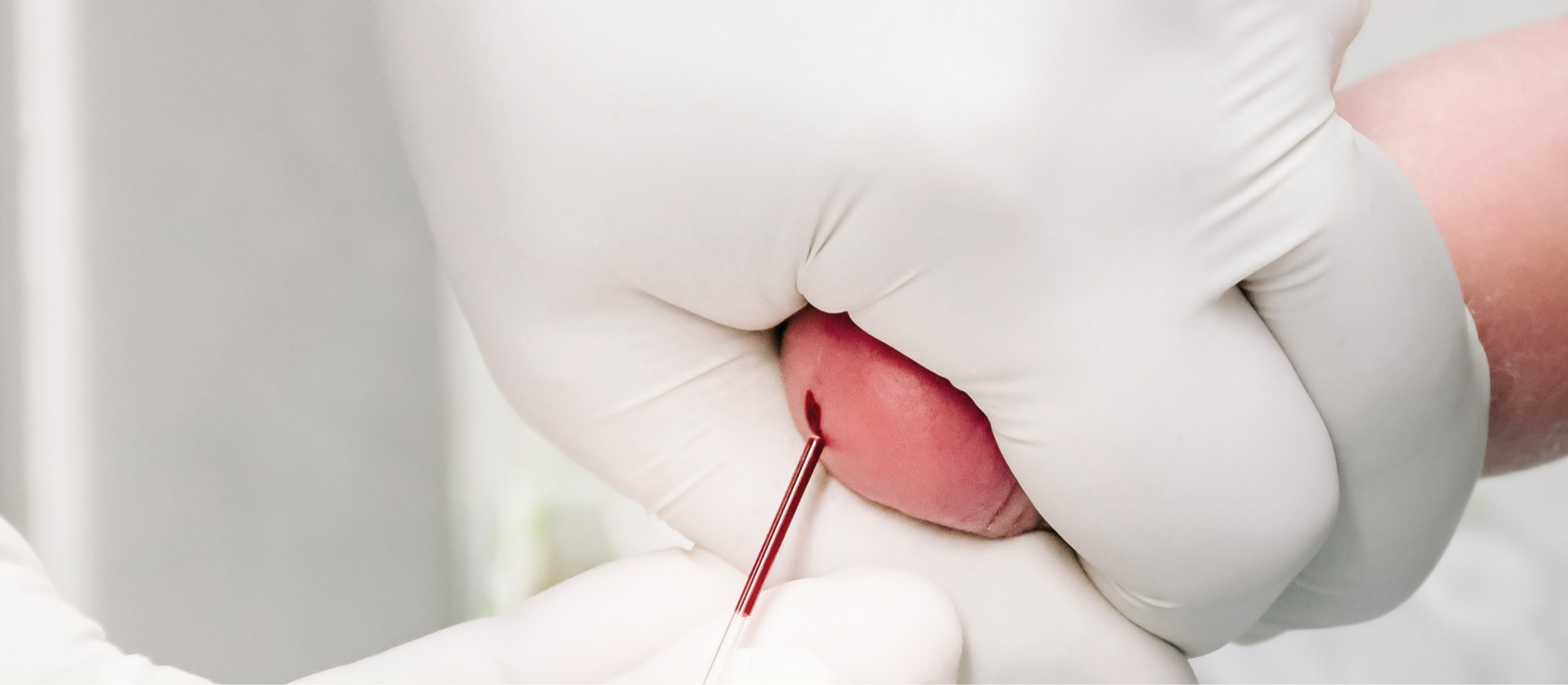
In recent years, KK Women’s and Children’s Hospital (KKH) is seeing an increasing number of paediatric patients presenting with NICCD. Paediatric patients with NICCD usually present with conjugated jaundice beyond two weeks of age, possibly accompanied by pale stool or poor weight gain. NICCD may not be detected by expanded newborn screening tests, which screen for IEM via a few drops of blood taken from the baby’s heel at birth, as derangement of the amino acid profile may not have yet taken place.
A simple but effective way to screen for citrin deficiency is to test for URS. Patients with citrin deficiency will test positive due to increased levels of galactose in the blood and the urine. A liver function test will also typically show raised bilirubin levels, consisting mostly of conjugated bilirubin and elevated alkaline phosphatase.
In addition, the patient’s plasma amino acid profile will usually indicate elevated levels of citrulline and amino acids such as threonine, methionine and tyrosine. Blood galactose levels will also be high but the activity of the GALT enzyme will be normal.
The diagnosis of NICCD is confirmed by performing sequencing and deletion / duplication analysis of the
SLC25A13 gene.
Management for patients with NICCD
In KKH, paediatric patients with NICCD are managed by a multidisciplinary team of doctors from the Genetics Service and Gastroenterology Service, dietitians and genetics resource nurses. Patients are started on a lactose-free soy milk or special amino acid-based formula, which helps to alleviate the secondary galactosemia.
They are also given medium chain triglyceride (MCT) oil supplements, which have been shown to help energy production in patient cases reported by Japanese researchers. Patients who present with liver failure are given supportive management whilst their liver function improves. Within a few weeks of treatment, patients demonstrate remarkable improvement in jaundice and liver function.
After they are discharged, patients with NICCD continue to receive support from the genetics resource nurses, and are followed up in the citrin deficiency clinic at KKH. Newly established in 2018, the specialised clinic is held once every three months, and enables each patient to meet with the multidisciplinary team during a single clinic session.
Early diagnosis of citrin deficiency is crucial in enabling timely intervention to prevent complications, and help patients to achieve optimal growth and development. Primary care providers play an important role in the early detection of infants who present with prolonged conjugated jaundice, and referring suspected cases for early tertiary assessment.
All infants with prolonged conjugated jaundice should have total and direct bilirubin tests performed. If the level of conjugated bilirubin is more than 20 μmol/L, the infant should be referred early to the paediatric gastroenterologist or paediatric jaundice clinic for workup.
Other causes of conjugated hyperbilirubinaemia, including anatomical causes such as biliary atresia and choledochal cyst, will need to be ruled out. The paediatric gastroenterologist will also perform infective and metabolic screening tests as clinically indicated.
Citrin deficiency is suspected if the metabolic workup reveals the abnormalities described above and is confirmed by genetic testing.
Research for the early detection of NICCD
Based on the current medical knowledge, it is not possible to predict the likelihood that an infant with NICCD will progress to develop complications later in life. The citrin deficiency team at KKH aims to pursue research into key factors determining the clinical presentation of citrin deficiency in neonates, and the efficacy of early intervention in altering the course of the condition.
Utilising genetic-based screening in Singapore as an adjunct tool in an upcoming research study, the team aims to detect citrin deficiency in newborn babies before the onset of symptoms. This will involve screening the newborns for common mutations in
SLC25A13 found in Singapore, using deoxyribonucleic acid (DNA) extracted from the drops of blood taken at birth for expanded newborn screening tests.
The research findings will be greatly beneficial to deepen the medical understanding of citrin deficiency, and enable the provision of more effective management and treatment for patients with the condition.

|
Dr Christina Ong, Head and Senior Consultant, Gastroenterology Service, KK Women’s and Children’s Hospital Dr Christina Ong graduated from the Imperial College School of Medicine, London, and received her post-graduate general paediatric and paediatric gastroenterology training at several major teaching hospitals in London. Dr Ong is currently on the specialist register for paediatric medicine and paediatric gastroenterology in Singapore and the United Kingdom, and has a special interest in inflammatory bowel disease, food allergies, gastrointestinal disorders, feeding difficulties and childhood nutrition. |

|
Dr Ting Teck Wah, Consultant, Genetics Service, KK Women’s and Children’s Hospital Dr Ting Teck Wah graduated from the National University of Singapore in 2006 and completed his paediatric medicine specialist training in 2014. His research interests are in the area of inborn errors of metabolism and genetics of neurodevelopmental delay. In 2017, Dr Ting completed his fellowship in the metabolic department of The Royal Children’s Hospital Melbourne, Australia. |
References: - Lu YB et al. Frequency and distribution in East Asia of 12 mutations identified in the SLC25A13 gene of Japanese patients with citrin deficiency. Journal of Human Genetics. 2005;50(7):338-46
- Bylstra Y et al. Population Genomics in South East Asia Captures Unexpectedly High Carrier Frequency for Treatable Inherited Disorders. Genetic in Medicine. In press.
- Hayasaka K et al. Treatment with lactose (galactose)-restricted and medium-chain triglyceride-supplemented formula for neonatal intrahepatic cholestasis caused by citrin deficiency. JIMD reports. 2012;2:37-44
- Saheki T et al. Citrin Deficiency. 2005 Sep 16 [Updated 2017 Aug 10]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2018.
|

