With the shift from inpatient to outpatient and home-based autologous haematopoietic stem cell transplantation, patients benefit from shorter inpatient stays, lower rates of nosocomial infections, and earlier return to independent functioning.
With the growing shift from inpatient to outpatient and home-based autologous haematopoietic stem cell transplantation, patients benefit from shorter inpatient stays, lower rates of nosocomial infections, and earlier return to independent functioning. The SingHealth Duke-NUS Transplant Centre shares how a shared-care model with general practitioners is envisaged in post-transplant monitoring and care in the near future.
INTRODUCTION
Haematological malignancies are on the rise worldwide, and Singapore is no exception. These increased incidence rates have been attributed to our ageing population, improvement in diagnosis and reporting and even environmental factors. In the 2018 Singapore Cancer Registry Report, lymphoid malignancies were ranked as the fifth most common cancer in males, and the sixth most common cancer in females.
AUTOLOGOUS HAEMATOPOIETIC STEM CELL TRANSPLANTATION
Autologous haematopoietic stem cell transplantation (auto-HSCT) is the cornerstone for treatment in relapsed B-cell lymphomas, and is also used as consolidative therapy in first-line treatment for T-cell lymphomas and multiple myeloma.
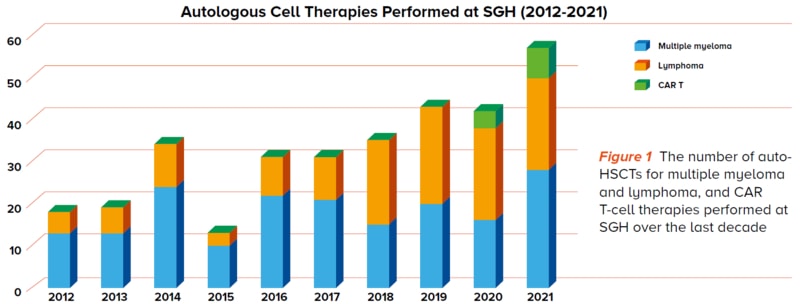
The increased incidence of haematological malignancies has also led to a steady increase in the number of auto-HSCTs performed at Singapore General Hospital (SGH) over the years (Figure 1).
A SHIFT FROM INPATIENT TO OUTPATIENT AND HOME-BASED AUTO-HSCT
An auto-HSCT comprises conditioning therapy for disease-directed cytotoxicity followed by infusion of stem cells previously collected from patients as a form of stem cell rescue.
Conditioning and stem cell infusion have traditionally been given in an inpatient setting, followed by a prolonged course of post-transplant monitoring, with a total stay of approximately three to four weeks. This is costly and also creates a significant strain on inpatient resources.
In a move to conserve inpatient resources, there has been a move towards outpatient and home-based auto-HSCTs.
Through forward planning and provision for access to outpatient and home-based medical and nursing support, conditioning regimens and post-transplant monitoring for stem cell transplants can be performed in the outpatient and home-based setting in a safe and effective manner.
THE INPATIENT AUTO-HSCT PATIENT JOURNEY
Auto-HSCTs are typically used in patients requiring high doses of chemotherapy, which are likely to damage the bone marrow. Healthy stem cells that were previously harvested from the patient are infused after the delivery of high-dose chemotherapy, to replace the damaged bone marrow.
The auto-HSCT journey typically involves three phases:
- Pre-transplant
- Peri-transplant
- Post-transplant
Pre-transplant
In the pre-transplant phase, patients will be admitted into the hospital. A central venous catheter will be inserted and patients will receive pre-transplant hyperhydration and conditioning chemotherapy. Their previously collected frozen stem cells will be reinfused back to them. The day of stem cell infusion is routinely called Day 0.
Peri-transplant
Patients will stay in an isolation room in the hospital throughout the peri-transplant phase, where their blood counts will nadir before blood count engraftment.
Neutropaenic phase
The main treatment-related morbidity and mortalities occur during the period of neutropaenia where patients are at risk of infective complications. The neutropaenic phase usually sets in from Day +3 to Day +5, and patients may remain neutropaenic for another seven to ten days before their stem cells engraft.
During this period, patients may develop neutropaenic fever, experience mucositis and/or develop significant gastrointestinal symptoms of nausea and vomiting, and abdominal cramps with severe diarrhoea.
The patients may require broad-spectrum intravenous antibiotics, intensive electrolyte repletion, transfusion of blood products and administration of opioids for oral pain control as well as other symptom-relieving medications.
Monitoring, support and recovery
The entire peri-transplant period typically ranges between 12-15 days. Whilst admitted, patients’ vital signs will be monitored closely, and strict intake and output charted accurately to guide intravenous fluid and electrolyte repletion.
In certain patients, parenteral nutrition may be necessary during this peri-transplant period. Some patients may experience temporary fragility and will require assistance in performing and completing some of their activities of daily living, such as toileting and ambulation.
In general, almost all patients recover well and can be discharged after two to four weeks of hospital stay.
Seemingly complex, the blood count nadir and engraftment periods for this form of auto-HSCT are fairly predictable. This predictability enables clinicians to schedule for the procedure in the outpatient or home environment.
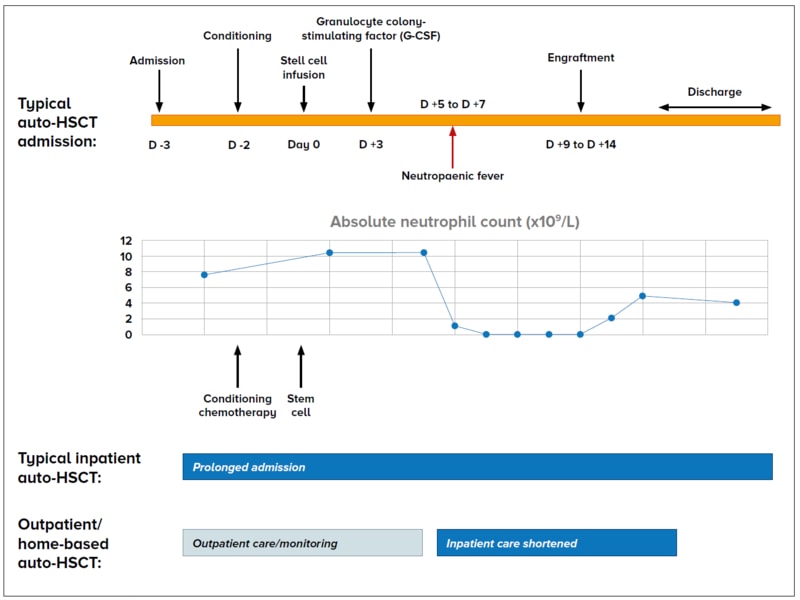
Figure 2 The typical patient journey for an inpatient and outpatient/home-based auto-HSCT
As shown in Figure 2, some patients can be selected to undergo outpatient or home-based auto-HSCTs. Benefits to patients In such situations, the conditioning chemotherapy and stem cell infusion are initiated in the outpatient setting. Patients are then monitored closely in the outpatient or home setting and may be admitted during the period of neutropaenia, or should the patient develop transplant-related complications. This shortens the inpatient stay period significantly. As compared to an inpatient auto-HSCT, outpatient and/or home-based auto-HSCTs may also reduce rates of nosocomial infections, which facilitates earlier return to independent functioning with improved reintegration into family and professional lives. Pre-transplant Initial pre-transplant interventions Patients undergoing the outpatient/home-based auto-HSCT may choose to receive their pre-transplant phase interventions either as an outpatient day admission at the SGH Haematology Centre, or as an inpatient hospital admission. - Patients who opt to receive treatment as an outpatient will go to the SGH Haematology Centre as scheduled to receive their pretransplant conditioning chemotherapy, as well as the reinfusion of their stem cells.
- Patients who choose to be admitted to the hospital to receive their pre-transplant treatment will be discharged from hospital after they receive their stem cell infusion.
Both groups of patients will be prescribed with prophylaxis medications to be taken strictly, as well as common symptom-preventive medications that can be consumed if required. Follow-up review and instructions Patients will be scheduled to return to the SGH Haematology Centre at least two to three times a week for blood tests. There will also be scheduled physical or virtual reviews with either the transplant physician or transplant advanced practice nurse. Patients are given clear instructions to return promptly to either the hospital emergency room after hours or the SGH Haematology Centre during office hours, if they develop a fever or feel unwell. Patients will also receive a memo with clear instructions to provide to the healthcare personnel who will be attending to them. Peri-transplant During the peri-transplant period at home, patients or their live-in caregivers are required to check their temperatures and blood pressures at least four times a day, or more frequently if required. They will be given clear instructions on a no-visitor policy, adherence to strict neutropaenic food precautions, maintenance of good personal hygiene, as well as the accurate charting of intake and output records. During this peri-engraftment period, patients commonly get readmitted to hospital for neutropaenic fever, severe diarrhoea or mucositis that affects their ability to consume fluids orally. Some patients may be discharged home from the hospital if well after three to five days of stay, while other patients may be discharged after blood count engraftment and resolution of symptoms. |
PATIENT SELECTION CRITERIA FOR OUTPATIENT / HOME-BASED AUTO-HSCT
When undergoing outpatient or home-based auto- HSCT, part of the care responsibilities will be on the patient and their caregiver(s). Hence, proper patient selection is important in ensuring a safe treatment journey.
To qualify, the patient must:
Be committed in taking all prescribed medications, adhering to medical and care advice, and returning to hospital according to the visit schedule and promptly if unwell
Have a dedicated 24-hour caregiver who will be with the patient, and is well and committed to accompanying the patient back to the hospital according to schedule, and promptly if the patient is unwell
Have a functional thermometer and blood pressure monitoring machine
THE GP’S ROLE: A VISION OF SHARED CARE
General practitioners (GPs) may progressively be involved in providing community or home-based care for such patients.
In the current model, patients return relatively frequently to the outpatient haematology clinic for symptom review, monitoring of blood counts and to receive electrolyte infusions or transfusions where necessary. Patients and caregivers often find travelling back to the hospital time-consuming, and it may also affect the patient’s rest in the acute post-transplant period.
We envision a shared-care model in the future, where GPs can partner with hospitalists to provide post-transplant monitoring.
In the shared-care model, GPs can accord patients with community-based or home-based care, such as reviewing a patient’s clinical symptoms and sending for laboratory investigations.
As part of the outpatient and home-based transplant team, they will be able to contact the transplant physician easily such that the patient can be seamlessly transferred back to the hospital to receive outpatient therapies or inpatient care, should the need arise.
FUTURE DEVELOPMENTS
There are also ongoing efforts looking into wearable vital monitoring devices that can be reflected in the hospital clinical charts, with appropriate thresholds set for the transplant physician or nurse to be notified. Such early warning systems can enable the team to reach out to the patients and advise early return to the hospital in a timely manner.
CONCLUSION
With a projected increase in the number of stem cell transplants and cellular therapies being performed for patients with haematological malignancies, there is now an accompanied increased need to pursue outpatient and home-based auto-HSCT.
Through close communication and monitoring of patients by a core group of transplant physicians, nurses, coordinators and community-based healthcare professionals, outpatient and home-based auto-HSCT enables patients to benefit by having their hospitalisations shortened, and having their post-transplant care take place in an environment they are most comfortable with.
Dr Chen Yunxin is a Consultant Haematologist at Singapore General Hospital. She specialises in the care of patients with multiple myeloma and lymphoproliferative disorders. She did her Health Manpower Development Plan on immunotherapy at the Memorial Sloan Kettering Cancer Center where she was involved in developing novel
cellular therapeutics for the treatment of multiple myeloma, as well as myeloma CAR T cell clinical trials. She works with a dedicated team of physicians and allied health professionals in the Haematopoietic Stem Cell Transplant Programme to deliver CAR T cells to patients as well as to develop outpatient transplant services.
Mr Jordan Hwang is an Advanced Practice Nurse (APN) with the Department of Haematology at Singapore General Hospital. He received his advanced training in adult cord blood transplantation nursing at the University of Minnesota Medical Center, USA in 2008; and APN-led services and haematopoietic stem cell transplantation training at the Princess Margaret Cancer Centre, Toronto, Canada.
To find out more about our transplant programmes, GPs can contact the SingHealth Duke-NUS Transplant Centre:
Tel: 6312 2720
Email: [email protected]
