Singapore’s first successful auditory brainstem implantation for a child below the age of seven years is paving the way for advancing intervention for paediatric hearing loss in Singapore.
The effort was led by
Associate Professor Henry Tan, Head and Senior Consultant, Department of Otolaryngology, in collaboration with
Dr David Low, Head and Consultant, Neurosurgical Service, KK Women’s and Children’s Hospital (KKH).
Six-year-old Natalie (not her real name) was found to have profound bilateral sensorineural hearing loss following universal newborn hearing screening in 2010. She was subsequently diagnosed with incomplete partition type 1 cystic cochleovestibular malformation of the right ear and a hypoplastic cochlea with dilated vestibule on the left ear.
“Despite the use of hearing aids from the age of two and auditory-verbal therapy, Natalie’s hearing did not improve. She was unable to develop any verbal output and was also dependent on sign language for very basic communication,” said A/Prof Tan.
Upon recommendation by doctors at KKH, she underwent a surgical auditory brainstem implantation in January 2017.
"The complexity of this procedure involves delicately accessing part of the brainstem and precisely positioning the implant. This is particularly challenging in younger patients as the anatomical structures are smaller and we are operating in a confined location with many critical structures in close proximity. We were fortunate to receive guidance from Professor Robert Behr from Fulda Clinic in Marburg, Germany," said Dr Low.
Six weeks after the surgery, Natalie’s implant was switched on and she began an intensive rehabilitation journey with support from her committed family. Results have been very positive.
“It was a challenging journey for Natalie and for us, as we were concerned about the risks of surgery and anxious about the results and potential benefits it would bring to her,” Natalie’s mother shared. “However, she did a great job coping with the surgery and recovery process in the hospital, and bounced back quickly.”
“Since her surgery, Natalie is able to respond when her name is called. She can also count from one to 10 without using sign language, and is even able to listen to music and dance to the beat,” Natalie's mother added.
“Following her successful auditory brainstem implantation, the improvement in Natalie's hearing will be greatly beneficial to improve her speech, language and neurocognitive development, as well as her psychosocial and learning skills, which are particularly important during her crucial years of rapid growth,” said A/Prof Tan.
“Following on, we hope to further develop KKH’s Paediatric Auditory Brainstem Implantation Programme, to help more children with hearing loss overcome the barriers of silence, achieve optimal outcomes and live full and meaningful lives,” added Dr Low.

A/Prof Henry Tan (right) consults with Dr David Low on a patient's condition.
Hearing loss in children
Hearing loss is the most common congenital and acquired sensory deficit among children. According to international reports, five out of 10,000 infants under two years are profoundly hearing impaired and unable to hear any sounds. Early onset profound hearing loss has been shown to have devastating consequences for the development of language and learning.
Annually, about one in 1,000 Singaporean infants are born with profound sensorineural hearing loss. Based on statistics at KKH, an estimated 12 infants are diagnosed with profound sensorineural hearing loss yearly.
Cochlear implant and auditory brainstem implant
The cochlear implant is the most successful neuro-prosthesis for restoring sensorineural hearing loss and provides meaningful sound and speech perception to paediatric patients worldwide.
Unfortunately, a small subset of patients with severe-to-profound sensorineural hearing loss cannot benefit from a cochlear implant, due to a small or absent cochlea or auditory nerve, or scarring of the inner ear due to infection or trauma.
Infants born without auditory nerves or cochlea are very rare, and comprise one to two cases per year. Patients who suffer from neurofibromatosis Type 2 (NF2) and have brain tumours leading to permanent damage in the auditory nerve are also not able to benefit from a cochlear implant. This spectrum of patients would depend on an auditory brainstem implant (ABI) as possibly the only hope of restoring their ability to hear.
An ABI is an electronic device that is surgically implanted to provide the patient with a sense of sound. It is typically an ideal intervention for patients with the following conditions:
- Severe cochlear malformation
- Complete ossification of cochlear
- Cochlear nerve hypoplasia
- Absent cochlear nerve
- Neurofibromatosis Type 2
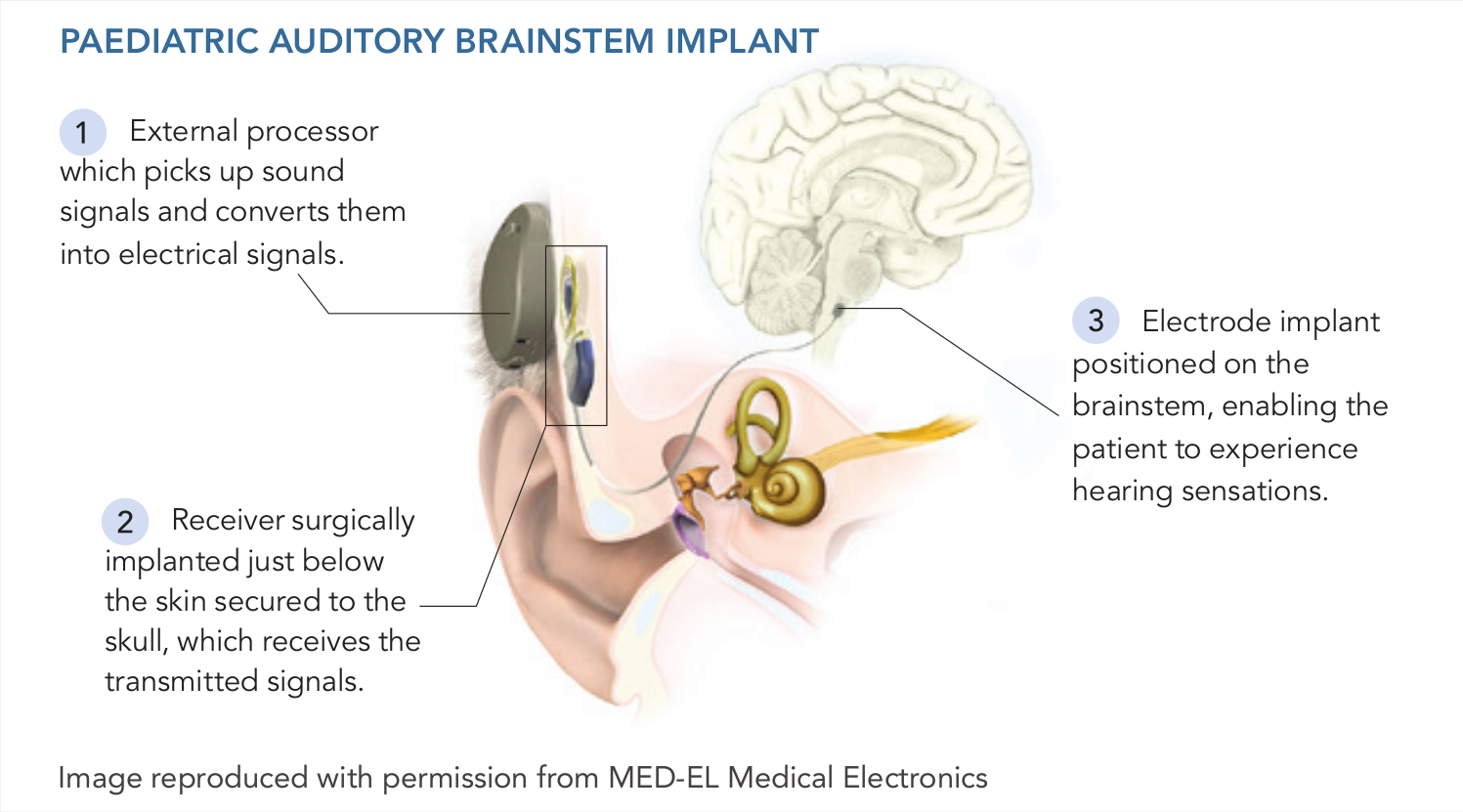
Utilising technology similar to a cochlear implant, the ABI directly stimulates the brainstem auditory pathway, bypassing both the cochlea and the eighth cranial nerve. It comprises two components – an external processor worn at the ear, which picks up sound signals and converts them into electrical signals; and a surgically implanted receiver positioned just below the skin secured to the skull, which receives the transmitted signals. The receiver is connected to an electrode implant positioned on the brainstem, enabling the patient to experience hearing sensations.
The ABI was originally developed to benefit patients with NF2, who had lost bilateral eighth cranial nerve function after undergoing surgery to remove vestibular schwannoma, a tumour which affects the eighth cranial nerve.
Post-implantation, these patients’ sound awareness showed improved performance over lip reading alone during face-to-face communication. However, speech understanding without visual cues (also known as ‘open-set’ speech recognition) was poor.
More recent results have seen high levels of open-set speech recognition in patients who had lost their eighth cranial nerve function from causes other than NF2. Post-ABI implantation, these patients, who did not have vestibular schwannoma, were able to recognise more than 50 percent of quietly spoken sentences and conduct conversations using the telephone.
Auditory brainstem implantation at KKH
At KKH, ABI surgery is jointly performed by a neurosurgeon and an otolaryngologist to access and expose the cochlear nerve nucleus via minimally-invasive keyhole craniotomy. An electrode is then microsurgically implanted in a targeted location identified via neurophysiological mapping techniques. Finally, a groove is created in the skull to house the receiver and connect it to the implanted electrode.
“Prior to the surgical procedure, the patient’s family receives rigorous counselling to educate them that the procedure alone does not provide an instantaneous cure nor enable the child to hear and perceive sounds similar to someone without hearing impairment,” said Dr Low.
“Post-surgery, the family would need to commit to regular auditory and speech rehabilitation sessions and practice sessions at home to maximise the chances of success of the treatment.”
Early detection key to successful intervention for hearing loss
Children with suspected hearing loss should be referred for tertiary assessment, which includes measurement of hearing thresholds and speech discrimination, as well as site-of-lesion detection – to diagnose and determine the type and degree of hearing loss.
Following diagnosis, the medical team can assess the impact of hearing loss on the child’s speech and language development, and conduct further tests to determine whether the child’s reduced hearing is indicative of a syndrome.
Rehabilitation and intervention measures can also be planned, which can include medical and surgical management, dispensing of hearing aids, or evaluation of the child for cochlear implants or ABI.
Note: A/Prof Henry Tan is also Clinical Associate Professor, Yong Loo Lin School of Medicine, National University of Singapore and Adjunct Associate Professor, Duke-NUS Medical School. Dr David Low is also Consultant, Department of Neurosurgery, National Neuroscience Institute, Program Director, SingHealth Neurosurgical Residency Program and Adjunct Assistant Professor, Duke-NUS Medical School.
Refer a patient:
Community healthcare practitioners can refer patients to the Department of Otolaryngology for assessment, by contacting the hospital at
+65 6294 4050. |

