Heart failure (HF) is a prevalent and chronic
condition that affects millions of people worldwide. Learn more from National Heart Centre Singapore (NHCS) Murmurs article.
Heart failure (HF) is a prevalent and chronic condition that affects millions of people worldwide. Thanks to medical advancements, significant progress has been made in understanding, diagnosing, and treating this complex condition.
By Asst Prof Iswaree Devi Balakrishnan, Consultant, Department of Cardiology
In this article, we will explore the diagnosis, updated classification, various aetiologies of HF, and the latest treatment options that are transforming the landscape of HF management.
HF in the Asian context
Compared to the rest of the world, prevalence of HF is higher in Singapore (4-5% vs 1-2% respectively)1.
Registry data of Asians with HF revealed two phenotypes unique to Southeast Asia, particularly in Singapore and Malaysia – the ‘lean diabetic’ group and the ‘metabolic’ group2. Patients with HF in the ‘lean diabetic’ group were characterised by high rates of diabetes despite a lower prevalence of obesity and had the worst clinical outcomes. Those in the ‘metabolic’ group were obese with higher rates of hypertension and diabetes. These distinct features seen in Asian patients underscore the impact of multi-morbidities and cardiometabolic dysregulation on HF, extending beyond left ventricular ejection fraction (LVEF: the percentage of blood pumped out of the left ventricle of the heart with each heartbeat). This highlights the significant influence of sedentary lifestyles, obesity, and inadequate management of risk factors like diabetes, hypertension, dyslipidaemia (imbalance of lipids), and tobacco smoking in HF genesis.
Another study examining Asian patients who were hospitalised for HF revealed notable disparities when compared to Western cohorts. Asian patients were relatively younger, presented with more severe clinical symptoms, had longer hospital stays, and a higher mortality rate3. These findings highlighted the need to address unique challenges in managing HF in the Asian cohort, through tailored interventions to improve outcomes.
What is HF?
HF is a clinical syndrome that occurs when the heart is not able topump as effectively as it should. Common signs and symptoms of HF include breathlessness, swelling of the feet and abdomen, fatigue and reduced effort tolerance. It is important to understand that the severity and manifestation of these symptoms can differ among individuals.
The most recent guidelines have established two primary classifications for HF that have overlapping components4.
Classification of HF by Stages
The first classification is based on the clinical stages of HF (Stage A-D). This classification recognises HF as a clinical syndrome that exists on a spectrum (figure 1).
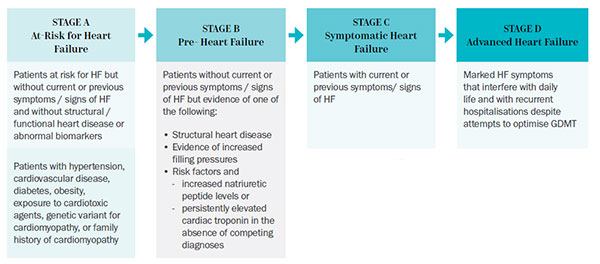
Figure 1: 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure
Classification of HF by LVEF
The second classification is based solely on LVEF (figure 2). This classification aims to guide the implementation of guideline-directed medical therapy (GDMT) since large clinical trials were primarily designed around LVEF criteria and carries prognostic significance. It is important to note that patients with normal LVEF can also experience symptoms of HF. This reaffirms the fact that HF is not exclusively based on LVEF alone.
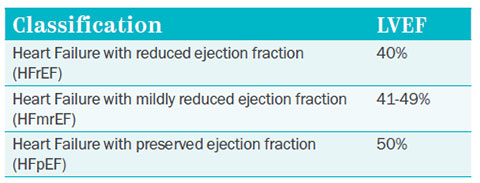
Figure 2: Adapted from 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure
Causes
HF is the eventual and downstream consequence that arises from different types of heart disease. One of the main causes of heart disease is coronary artery disease, which involves the buildup of atherosclerotic plaques leading to heart attacks. This often leads to heart failure with reduced ejection fraction (HFrEF). Inadequately managed risk factors such as hypertension, diabetes, dyslipidaemia, and unhealthy lifestyle choices including tobacco smoking, sedentary behaviour, and unhealthy diet contribute to accelerated atherosclerosis (plaque buildup), can increase the risks of heart attacks and HF.
Even without experiencing heart attacks, traditional risk factors like uncontrolled hypertension, diabetes, and obesity can contribute to the development of HF. This occurs due to cardiometabolic dysregulation, where these risk factors disrupt the normal functioning of the heart. It typically results in heart failure with preserved ejection fraction (HFpEF), a condition predominantly seen in those aged 65 years and above5.
Other less common causes of HF include valvular heart disease, arrhythmias (irregular heartbeat), cardiotoxicity meditated by cancer therapeutics or substance abuse (e.g. alcohol), myocarditis
(inflammation of the heart muscles), genetic cardiomyopathy (heart muscle disease), stress-induced cardiomyopathy, peripartum cardiomyopathy and infiltrative heart disease (e.g. amyloidosis, sarcoidosis)4. Ascertaining the specific aetiology of HF requires a thorough evaluation.
Diagnosis
HF often co-exists with other medical conditions and cannot be diagnosed with a single test. To diagnose HF, a thorough process is followed. This involves gathering a detailed medical and family history, conducting a physical examination, performing blood tests, and depending on the specific clinical situation, cardiac imaging (e.g. echocardiography, cardiac magnetic resonance imaging) and coronary artery assessment (e.g. coronary angiogram). After a comprehensive evaluation, a diagnosis of HF and its aetiology can be established. With this in hand, a treatment plan can be tailored to address the individual's condition effectively.
How to Manage HF?
Management options for HF include risk factor and lifestyle modification, guideline-directed medical therapy (GDMT), and in some cases device therapy, ventricular assist device (VAD) and/or
heart transplant.
Risk Factor Screening and Lifestyle Modification
The serious implications of cardiovascular risk factors in the genesis of HF have been previously discussed. Regular age-appropriate screening is crucial to identify these risk factors, as they are often unrecognised. Early detection through screening enables timely intervention and treatment, reducing the incidence of HF. In addition, a heart-healthy lifestyle through dietary improvements, regular exercise and stress management is key in preventing HF decompensations.
Guideline-Directed Medical Therapy (GDMT)
GDMT for HF is primarily based on LVEF, with specific treatments tailored to the underlying cause.
The greatest body of evidence exists for patients with HFrEF where GDMT has significantly improved survival and prognosis. In the last decade, the introduction of novel medical therapies has significantly transformed clinical practice and established the four pillars of GDMT for HFrEF4. These include angiotensin-converting enzyme inhibitors (ACE-I) or angiotensin receptor/ neprilysin inhibitors (ARNI), beta-blockers, mineralocorticoid receptor antagonists (MRA), and sodium-glucose cotransporter-2 inhibitors (SGLT2I). Second-line therapies targeting alternative pathways to improve outcomes in HFrEF include ivabradine and vericiguat.
In the context of HFmrEF and HFpEF, where symptomatic treatment with diuretics was previously the main approach, the emergence of SGLT2I has made a breakthrough with significant reduction in HF hospitalisations and cardiovascular deaths.
Device Therapy in HF
In patients with HFrEF who do not show sufficient improvement to GDMT, CRT (cardiac resynchronisation therapy) may be considered. This treatment aims to enhance the heart’s pumping efficiency and alleviate heart failure symptoms. Additionally, for individuals who are at high risk of life-threatening arrhythmias, an implantable cardioverter defibrillator (ICD) plays a crucial role in reducing the risk of sudden cardiac death4.
In cases of severe secondary mitral regurgitation due to HFrEF, despite GDMT and CRT (if applicable), transcatheter edge-to-edge mitral valve repair may be considered as a potential intervention to prevent the progression of HF6.
Ventricular Assist Device (VAD) and Heart Transplant
In some cases, patients with chronic HF may reach an advanced stage where symptoms become severe and they no longer respond to medical therapies and/or device therapies. For such individuals, a VAD can be considered. A VAD is a mechanical device that assists in pumping blood throughout the body. It has demonstrated benefits in improving symptoms and reducing mortality in these patients4. However, VAD implantation is a major surgical procedure that requires meticulous post-VAD care and strong commitment from the patient and their family. Therefore, a multidisciplinary team is necessary to evaluate both the medical and psychosocial aspects of the patient to ensure appropriate selection and achieve the best possible outcomes.
Heart transplantation is another option for patients with advanced HF to improve survival4. Similar to VAD candidacy assessment, a thorough evaluation process is imperative to identify suitable candidates who have the highest potential for favourable outcomes with a heart transplant. This rigorous process is necessitated by the scarcity of donor hearts. Eligible patients are placed on a waiting list and informed when a suitable donor heart becomes available.
As of 2023, over 90 heart transplants have been carried out at NHCS, the only healthcare institution in Singapore that carries out heart transplantations.
Advance Care Planning and Palliative Care
Even though HF treatment has improved, with the increase in life expectancy, the burden of heart failure is expected to rise in ageing societies like Singapore. Integrating advance care planning and palliative care into management plan becomes crucial to provide holistic care in conjunction with medical treatment. These initiatives address the unique needs of patients and their families, ensuring comprehensive support and enhancing quality of life.
Further Enhancements in HF Management Needed
Significant advancements have been made in understanding HF epidemiology, pathophysiology, diagnosis, medical treatment, device therapy, and palliative care. However, further enhancements in HF management are still needed. Continued focus on research and development in addressing the complexities of HF care holds tremendous potential. This dedicated pursuit will pave way for the adoption of more personalised and effective treatments, ultimately optimising health outcomes. By fostering innovation and collaboration within the community at large, we can cultivate a sense of renewed hope and work towards a brighter future in managing HF.
This article is from Murmurs Issue 45. Click here to read other articles or issues.
References
- Lam CSP. Heart failure in Southeast Asia: facts and numbers. ESC Hear Fail. 2015;2(2):46-49.doi:10.1002/ehf2.12036
- Tromp J, Tay WT, Ouwerkerk W, et al. Multimorbidity in patients with heart failure from 11 Asian regions: A prospective cohort study using the ASIAN-HF registry. PLoS Med. 2018;15(3):1-22. doi:10.1371/journal.pmed.1002541
- Atherton JJ, Hayward CS, Wan Ahmad WA, et al. Patient characteristics from a regional multicenter database of acute decompensated heart failure in Asia Pacific (ADHERE International-Asia Pacific). J Card Fail. 2012;18(1):82-88. doi:10.1016/j.cardfail.2011.09.003
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(17):e263-e421. doi:10.1016/j.jacc.2021.12.012
- Schiattarella GG, Hill JA. Cardiometabolic HFpEF: Mechanisms and Therapies. CardioMetabolic Syndr J. 2021;1(2):117. doi:10.51789/cmsj.2021.1.e18
- Pibarot P, Delgado V, Bax JJ. MITRA-FR vs. COAPT: Lessons from two trials with diametrically opposed results. Eur Heart J Cardiovasc Imaging. 2019;20(6):620-624. doi:10.1093/ehjci/jez073
