For patients with chronic kidney disease, general practitioners can help with long-term management, treat common symptoms, and identify when specialist referral is needed. SingHealth Duke-NUS Supportive & Palliative Care Centre shares more.
General practitioners (GPs) are often the first port of call when patients with chronic kidney disease see a deterioration in kidney function – placing them in prime position to guide the patient journey and decision making process. Read all about how GPs in the primary care setting can start important conversations on long-term management, treat common symptoms, and identify when specialist referral for renal supportive care would be beneficial.
CHRONIC KIDNEY DISEASE
Increasing disease burden in Singapore
The burden of chronic kidney disease (CKD) among
the Singaporean population has been increasing in
recent years, contributed to by diabetes and an ageing
population. Diabetic kidney disease is the main cause
of kidney failure for patients on dialysis in Singapore.
The number of patients newly diagnosed with stage
5 chronic kidney disease (CKD5), as defined by an
estimated glomerular filtration rate (eGFR) of < 15 ml/min/1.73m2, serum creatinine ≥ 500 μmol/L or initiation of renal replacement therapy, has increased from
1,586 in 2011 to 2,079 in 2019.1
Management of advanced chronic kidney disease
Patients with advanced CKD (CKD stage 4 to 5) are
assessed by renal teams through a process of shared
decision making, to determine a long-term treatment
plan which may include:
While dialysis confers a significant survival advantage
for patients with CKD5 in general, this advantage is lost in patients who are older (> 80 years old)2, with poor functional status and/or a high comorbidity burden. Some patients may find dialysis to be burdensome and
experience unacceptable reduction in their quality
of life.
Therefore, it is important to recognise this group of
patients and consider whether a supportive care
approach would be more beneficial.
General practitioners (GPs) play an important role
in the holistic management of patients with CKD.
This will be even more so with the Ministry of Health's
recommendation for each household to have their
own family doctor from 2023.
This article shares the concept of renal supportive
care and explores how GPs may support their patients
who have advanced CKD.
WHAT IS RENAL SUPPORTIVE CARE?
Renal supportive care (RSC) is a clinical approach that aims to improve the quality of life for patients with advanced CKD by integrating palliative care principles,
knowledge and skills into routine renal care.
RSC can be provided at any part of the patient journey,
including for those who choose dialysis (Figure 1).
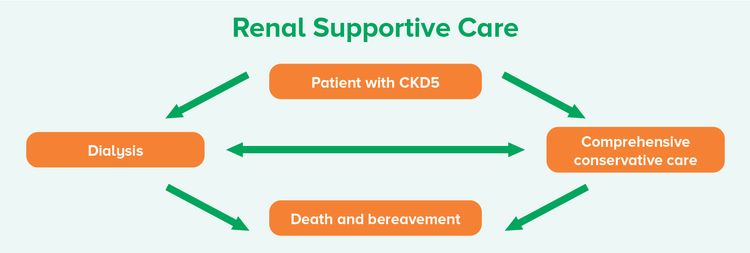
Figure 1 Renal supportive care encompasses all parts of the CKD5 patient journey3
Comprehensive conservative care4-5 is a holistic patient-centric approach which supports patients who opt for non-dialytic therapy. For patients who are unlikely to benefit from dialysis or kidney transplantation as a treatment choice, comprehensive conservative care is an option that should be provided. Patients are assured of
continued medical care so they do not go away with the notion that ‘nothing can be done’, and receive treatment
plans that are aligned with their priorities and values.
Holistic patient-centered care for patients with CKD5 which includes: Interventions to delay progression of kidney
disease and minimise risk of adverse events or
complications Shared decision making Active symptom management Detailed communication, including advance care planning (ACP) Psychological and spiritual care Culturally-aligned social and family support
Comprehensive conservative care does not include dialysis. |
Table 1 Definition of comprehensive conservative care4-5
CASE STUDY
Background
Mdm T is an 80-year-old woman with CKD5 secondary to
diabetic kidney disease and concomitant hypertension, hyperlipidaemia and gout. She was referred by her
nephrologist to the RSC clinic for symptom management
and psychosocial support.
Laboratory results:
• eGFR 7ml/min
• Creatinine 492 μmol/L
• Urea 28.4 mmol/L
• Potassium 3.8 mmol/L
• Bicarbonate 22.4 mmol/L
• Albumin 37 g/L
• Calcium 2.63 mmol/L
• Phosphate 1.63 mmol/L
• Hb 11.0 g/dL
• Transferrin saturation 31.3%
Symptom and psychosocial assessment
She had mild fatigue, low appetite and poor sleep. There
were no symptoms of uraemia or fluid overload. She had
low mood due to her husband’s cognitive decline and
behavioural issues. While her mood gradually improved
following her husband’s admission to a nursing home,
her family still felt guilty about the decision.
Treatment decision and goals of care discussion
She was aware of her CKD5 status and the potential for
complications. She readily stated that she did not want
dialysis as she was old and life prolongation was not
meaningful to her. She had loss of weight but was not
keen on further investigations.
She preferred to focus on comfort and symptom control,
but was willing to be hospitalised for treatment if deemed beneficial. She decided on inpatient hospice as her
preferred place of care and death when her condition
deteriorated.
Management plan
Her medication list was reviewed and adjusted,
taking into consideration her symptoms, pill burden
and whether she would have the time to benefit from
taking the medications.
As her mood was improving, she did not require
antidepressants.
She was planned for referral to Assisi Hospice Day Care.
The RSC team planned to follow up on Mdm T and
her family’s coping during subsequent appointments
Case Progress
SEP 2019 | • eGFR 7 ml/min
• First consult at RSC clinic |
|---|
NOV 2019 | • eGFR 5 ml/min
• Family had brought her on an overseas holiday; mood was better
• Had mild exertional dyspnoea and slightly worse appetite
• Given standby mist morphine 2.5 mg Q8H PRN for dyspnoea
• Not keen on hospice day care; referred to community palliative nursing |
|---|
JAN 2020 | • eGFR 5 ml/min
• On follow-up with community palliative nursing
• Condition was stable; mood was good
• Referred to Assisi Home Hospice in view of declining GFR |
|---|
SEP 2020 | • eGFR 3 ml/min
• Admitted to Singapore General Hospital (SGH) for fluid overload and anaemia
• Treated with intravenous iron and recormon
• Frusemide dose increased |
|---|
OCT 2020 | • eGFR 3 ml/min
• Developed more fluid overload and uraemic symptoms
• Still able to manage at home and declined admission to inpatient hospice
• Given oral haloperidol 0.5 mg Q8H PRN for nausea
• Explored her needs and coping with her deterioration |
|---|
NOV 2020 | • eGFR 3 ml/min
• Much more fatigued, Hb 6.2
• Admitted to SGH and transfused as she was still functionally well and living alone; felt better after transfusion |
|---|
DEC 2020 | • Admitted to Assisi Inpatient Hospice
• Died in end December 2020 |
|---|
SGH Low Clearance Clinic and Renal Supportive Care Clinic
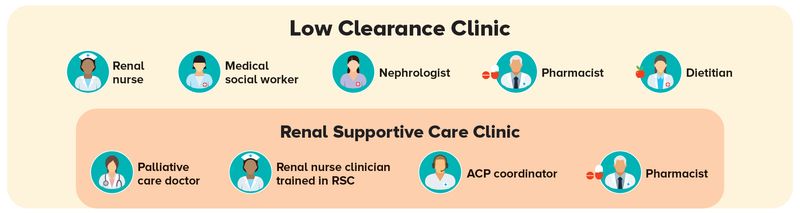
The SGH Department of Renal Medicine set up the
multidisciplinary Low Clearance Clinic (LCC) in
August 2015 with the aim of better preparing CKD
patients for end-stage kidney failure and their long-term
treatment plan.
Patients with GFR of < 20 ml/min are managed by
a multidisciplinary team consisting of nephrologists,
advanced practice/specialist nurses, dietitians,
pharmacists, social workers and renal coordinators/case managers.
The Renal Supportive Care Clinic was started in August 2016 and is embedded in the multidisciplinary
LCC service. The RSC clinic team consists of a
palliative care consultant, renal nurse clinician with
training in RSC, ACP coordinator and pharmacist.
Presently, patients who choose comprehensive
conservative care with eGFR < 9 ml/min or who have significant supportive and palliative care needs
such as poor symptom control and psychosocial
issues are referred for a RSC clinic consult.
WHAT WE DO AT THE RSC CLINIC
After every RSC session, the team participates in a multidisciplinary team meeting to discuss and identify
‘worry board’ cases who need closer follow-up or interventions. The RSC team also participates in the
multidisciplinary haemodialysis rounds to provide supportive care input for complicated dialysis patients.
Symptom assessment
and management | Manage symptoms of CKD such as those from fluid overload and uraemia Manage other symptoms such as pain, constipation, etc. Monitor for worsening symptom burden and functional decline Prognostication
|
Optimised medical
management of CKD
and comorbidities | Chronic disease management Discussion with nephrologist as needed Dietitian support in the same setting
|
Psychosocial assessment
and support | - Dedicated renal medical social worker to assess patient on the same day
if needed
|
Medication review
and deprescribing | - Pharmacist to help with medication reconciliation, counselling and
collaboration on deprescribing
|
Support for family
and caregivers | - Referrals to appropriate community partners such as community nurses or
hospice services
|
Advance care planning | - Referrals to appropriate community partners such as community nurses or hospice service
|
Table 2
What GPs Can Do in Primary Care
GPs who have been following up on their patients with CKD are often the first port of call when their kidney
function begins to decline. Having built strong doctor-patient relationships, GPs are well-placed to begin the conversation about their patients’ values and priorities. This will help patients to navigate the decision making process when it comes to considering whether dialysis or comprehensive conservative care is right
for them.
1. Identify patients with
CKD5 or advancing CKD | |
2. Review treatment plan | - Review medications to optimise chronic disease management and
minimise polypharmacy, by stopping medications with limited benefit
|
3. Discuss treatment preferences and
goals of care | Discuss the patient’s values and priorities, and whether interventions such as dialysis would achieve their desired life goals Consider discussing and completing an ACP
|
4. Consider referral to a palliative care specialist
if complex symptoms or
psychosocial issues present | - Patients who are experiencing increasing distress from symptoms or complex psychosocial issues may benefit from assessment and multidisciplinary management from a palliative care specialist
|
5. Discuss the long-term
care plan if decided on
non-dialytic treatment
| Review their psychosocial background and care setting Pre-empt the patient and/or their family on the potential need for hospice services Explore (if relevant) whether the patient and their family have planned for a Lasting Power of Attorney (LPA) and will
|
6. Refer to hospice services
if deteriorating on
conservative care
| |
Table 3
Symptom | Prevalence | Symptom | Prevalence |
1. Fatigue | 71% | 6. Insomnia | 44% |
2. Pruritus | 55% | 7. Anxiety | 38% |
3. Constipation | 53% | 8. Nausea | 33% |
4. Anorexia | 49% | 9. Restless legs | 30% |
5. Pain | 47% | 10. Depression | 27% |
Table 4
Symptom | Management |
Fatigue | Screen for causes of fatigue (e.g., uraemia, fluid overload, anaemia, sleep apnoea,
other comorbid conditions such as heart failure) Iron supplementation and referral to a renal specialist for erythropoiesis-stimulating
agents Advise on non-pharmacological measures including energy conservation strategies
and exercise
|
Anorexia | Screen for depression, taste disorders, constipation or diarrhoea Nutritional counselling and supplementation as required Review medications for polypharmacy and adverse effects Review for and treat nausea and/or dyspepsia
Consider antidepressants such as mirtazapine if there is concomitant depression Presently, there is no evidence for the use of appetite stimulants such as megestrol in
CKD5 patients on conservative management
|
Pruritis | Assess for and treat dermatological causes such as eczema and xerosis with topical
emollients Control calcium and phosphate levels Refer to a renal specialist for treatment of hyperparathyroidism Systemic therapy with gabapentin/pregabalin or mirtazapine Start at lower doses particularly in elderly patients, and monitor for adverse effects Starting doses: Gabapentin 100 mg ON, maximum 300 mg/day Pregabalin 25 mg ON, maximum 100 mg/day Mirtazapine 7.5 mg ON
Night dose of antihistamine (e.g., hydroxyzine) for light sedation to reduce scratching
|
Pain | - Assess and treat cause of pain
- Avoid nephrotoxic medications such as nonsteroidal anti-inflammatory drugs (NSAIDs)
- Use weak opioids such as tramadol with caution, limiting dosage to a maximum of
100 mg/day
- Consult a palliative care physician for advice if strong opioids are needed
|
Table 5
Difficult symptom burden and treatment Challenges in decision making for long-term treatment plan, with complex clinical situations
or psychosocial issues Multidisciplinary team support required For assistance in ACP and end-of-life care
|
Referral process
Currently, the RSC clinic is only open to referrals for
patients known to the Department of Renal Medicine,
SGH.
If you have an advanced CKD patient who may
benefit from a consult with a palliative care specialist,
you may contact the SGH GP Appointment Hotline
at 6326 6060 to make an appointment with the
Internal Medicine Supportive and Palliative Care
Service, which provides specialist palliative care
support for the RSC clinic.
GPs who would like more information may contact
the following palliative care physicians in the RSC
team:
Dr Natalie Woong:
[email protected]
Dr Lee Guozhang:
[email protected]
CONCLUSION
The burden of chronic kidney disease in our population is significant. With a better understanding of renal
supportive care, GPs can play an important part in their patients' decision making process and journey by starting
the conversation on long-term CKD management, reviewing chronic disease management and considering
specialist referral for shared care.
REFERENCES
Singapore Renal Registry Annual Report 2020
Verberne, W. R., Geers, A. B., Jellema, W. T., Vincent, H. H., van Delden, J. J., & Bos, W. J. (2016). Comparative Survival among Older Adults with
Advanced Kidney Disease Managed Conservatively Versus with Dialysis. Clinical journal of the American Society of Nephrology : CJASN, 11(4), 633–640. https://doi.org/10.2215/CJN.07510715
Hole, B., Hemmelgarn, B., Brown, E., Brown, M., McCulloch, M. I., Zuniga, C., Andreoli, S. P., Blake, P. G., Couchoud, C., Cueto-Manzano, A. M.,
Dreyer, G., Garcia Garcia, G., Jager, K. J., McKnight, M., Morton, R. L., Murtagh, F., Naicker, S., Obrador, G. T., Perl, J., Rahman, M., … Caskey, F. J.
(2020). Supportive care for end-stage kidney disease: an integral part of kidney services across a range of income settings around the world. Kidney international supplements, 10(1), e86–e94. https://doi.org/10.1016/j.kisu.2019.11.008
Davison, S. N., Levin, A., Moss, A. H., Jha, V., Brown, E. A., Brennan, F., Murtagh, F. E., Naicker, S., Germain, M. J., O'Donoghue, D. J., Morton, R. L.,
Obrador, G. T., & Kidney Disease: Improving Global Outcomes (2015). Executive summary of the KDIGO Controversies Conference on Supportive
Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney international, 88(3), 447–459. https://doi.org/10.1038/ki.2015.110
Murtagh, F. E., Burns, A., Moranne, O., Morton, R. L., & Naicker, S. (2016). Supportive Care: Comprehensive Conservative Care in End-Stage Kidney
Disease. Clinical journal of the American Society of Nephrology : CJASN, 11(10), 1909–1914. https://doi.org/10.2215/CJN.04840516
Murtagh, F. E., Addington-Hall, J., & Higginson, I. J. (2007). The prevalence of symptoms in end-stage renal disease: a systematic review. Advances in chronic kidney disease, 14(1), 82–99. https://doi.org/10.1053/j.ackd.2006.10.001
Dr Natalie Woong is a Consultant at the Department of Internal Medicine, Singapore
General Hospital. She is an accredited palliative care specialist and works with the
Department of Renal Medicine as part of the Renal Supportive Care team to provide care
for patients with advanced kidney disease.
Acknowledgements
Dr Lee Guozhang
Assoc Prof Jason Choo
Clin Asst Prof Alethea Yee
Clin Asst Prof Peh Tan Ying
Dr Kwek Jia Liang
GPs can call the SingHealth Duke-NUS Supportive & Palliative Care Centre for appointments at the following hotlines:
Singapore General Hospital: 6326 6060
Changi General Hospital: 6788 3003
Sengkang General Hospital 6930 6000
KK Women’s and Children’s Hospital: 6692 2984
National Cancer Centre Singapore 6436 8288
National Heart Centre Singapore 6704 2222
National Neuroscience Institute 6330 6363
