There is a rising incidence of food allergies among children, with the current local prevalence estimated at about five per cent. Most food allergies start during early childhood. Common allergens include egg, cow’s milk, peanuts and tree nuts, shellfish, wheat, soy and fish.
The KK Women’s and Children’s and Hospital (KKH) Allergy Service has observed:
- 3X the number of children with positive skin prick test results for egg, cow’s milk, peanut and shellfish – the top four food allergens – from 2012 to 2022.
- Close to 2.5X visits to the KKH Children’s Emergency due to food-induced anaphylaxis (severe, potentially life-threatening allergic reaction) from 12.6 to 30.1 per 100,000 person-years between 2015 and 20221.
Severity of food allergy reactions are unpredictable
Food allergic reactions vary in severity, from mild to moderate symptoms (such as hives, oral itching, facial swelling, acute vomiting, abdominal pain and diarrhoea) to severe reactions or anaphylaxis that affect airway, breathing or consciousness. The severity of a reaction is unpredictable as it depends on multiple factors, including the amount of allergen ingested or exposed to, and the presence or absence of co-factors such as illness, exercise, and sleep deprivation, among others.
It is important to understand that allergy test results (including skin prick tests or food-specific IgE levels) do not indicate the severity of food allergic reactions. A child who has previously experienced only mild reactions can still develop severe anaphylaxis if exposed to a larger amount of allergen or when co-factors are present.
Severe food allergy reactions can be life-threatening and require immediate response and self-treatment.
Therefore, it is essential for patients and their families to recognise anaphylaxis symptoms (as outlined in Annex B of the KKH Allergy Action Plan), administer swift self-treatment (EpiPen if available), or seek immediate medical attention to ensure their children's safety. During anaphylaxis, time is critical, as prompt administration of adrenaline can prevent refractory and severe reactions.
Food intolerance is not an allergy
While food intolerances and food allergies may present with similar symptoms, there are key differences between the causes, severity of symptoms and management options (Table 1).
Food intolerances typically affect the digestive system. Children suspected to have food intolerances should see a general practitioner or paediatrician, for accurate diagnosis and dietary guidance. If food allergy is suspected, evaluation by an allergist will be required.
Table 1. Differentiating food allergies from food intolerances
Food allergies
|
Food intolerances
|
Cause:
- Caused by the immune system mistakenly treating harmless proteins in certain foods as a threat.
Symptoms:
- Mild to moderate allergic reactions can include itchy rashes (hives), itch in the mouth, facial swelling, acute vomiting, abdominal pain or diarrhoea.
- Severe and potentially fatal reactions or anaphylaxis can occur where the airway, breathing and/or consciousness is affected.
Management:
- Strict allergen avoidance is the mainstay of management, with oral immunotherapy as a potential treatment option in select cases.
- Children with food allergies are also taught self-treatment using intramuscular adrenaline for anaphylaxis, following incidental allergen exposure.
| Cause:
- Does not involve the immune system, typically relates to difficulties digesting certain foods.
- A common cause of food intolerance is due to the lack of lactase to digest lactose (a milk sugar) in cases of lactose intolerance.
Symptoms:
- Symptoms are usually much slower to develop and often require larger amounts of the food to result in symptoms such as bloating, cramps, diarrhoea or nausea. These are typically not life-threatening.
Management:
- Can be managed with dietary adjustments or enzyme supplements; may be able to eat small amounts.
|
Toolkit for healthcare professionals in managing food allergies
-
Educate caregivers against “over-diagnosing” to prevent unnecessary food avoidance
In recent years, unvalidated “allergy tests” such as blood testing for food IgG levels have been surfacing online. Primary care physicians and general paediatricians should educate caregivers that such tests do not confirm the diagnosis of an immediate food allergy and are not useful in making a diagnosis of delayed food allergies or intolerances.
It is also important to note that a positive skin prick or food-specific IgE test result only confirms sensitisation and not clinical allergy. Children can have a positive IgE to a food but still be clinically tolerant (“false positive test”). Caregivers should be cautioned against over-diagnosing food allergy and discouraged from the use of unvalidated, inaccurate tests. These can lead to unnecessary food restrictions or avoidance, which will impact a child’s nutritional status, psychosocial and emotional well-being.
Children with “self-diagnosed” or perceived food allergies that result in food avoidances should be offered a referral to a paediatric allergist for evaluation.
-
Community healthcare professionals are encouraged to be familiar with the World Allergy Organization’s diagnostic criteria for anaphylaxis (Annex A) and immediate first-line treatment using intramuscular adrenaline.
- Know the dose (and correct concentration) of adrenaline for prompt treatment.
- Attach a dosing card to the e-trolley of the clinic, for quick and easy reference.
- Avoid delay in administration of adrenaline which is a known prognostic factor for refractory and severe anaphylaxis.
-
Frequently Asked Questions about food allergies by parents and caregivers
Preconception and antenatal
|
Question: What can I do to reduce the chances of allergy in my baby before or during pregnancy?
Response: There is currently no consistently proven strategy for pregnant mothers to reduce the chances of allergies in their newborn. There is also currently no recommendation for the avoidance of foods during pregnancy.
A woman’s state of health before pregnancy is important for the baby’s subsequent well-being. Mothers should maintain a healthy lifestyle before and during pregnancy by adopting a healthy diet, having an ideal weight and adequate exercise and sleep.
|
Question: Can I be tested antenatally to detect whether my baby is at risk of having an allergy?
Response: Allergy tests in the mother are not recommended or used to predict a baby’s allergies. Positive allergy tests in the mother do not necessarily mean that the baby will have allergies or allergic diseases.
|
Early childhood to adolescence
| Question: Should I pre-emptively have my baby tested for allergies “in case” an allergy reaction happens when he/she gets older?
Response: Allergy tests should only be performed if there is suspicion of food allergy, after a detailed history is obtained by the allergist. Positive skin prick or food-specific IgE tests only confirm sensitisation and not clinical allergy. Allergy tests are best performed by specialists who are trained to interpret them.
|
Question: Should I delay weaning to reduce my baby’s exposure to potential allergens?
Response: Breastfeeding for the first six months of life is recommended for all babies for all its benefits. Weaning can start at the appropriate time between four and six months. All foods should be given in a manner that the child can safely take without delaying introduction of allergenic foods beyond one year of life.
|
Question: Will my child “outgrow” his/her food allergy naturally as they get older?
Response: Children with egg and milk allergy tend to outgrow their food allergy with age. Whereas children with peanut or shellfish allergy are less likely to outgrow their allergy, and for those who do, it may take a longer period of time.
Food allergies that children have outgrown tend not to recur. The main food allergy that tends to occur later in life is shellfish allergy.
|
Interventions for food allergy in children
At KKH, children with food allergies are managed by a multidisciplinary team consisting of paediatric allergy specialists, gastroenterologists, specialist allergy nurses and dietitians.
Currently, the mainstay of management for food allergy is strict allergen avoidance, counselling to recognise and manage allergic reactions from accidental exposures. An individualised Allergy Action Plan (Annex B) is provided to food allergic patients.
- Following a confirmed diagnosis, families are educated on the food to avoid, especially learning to read food labels, as the allergen may be hidden within ingredients.
- Families are advised on means to keep themselves safe from accidental exposures in the home, school and community. These include regular counselling to prompt self-treatment of inadvertent allergic reactions, such as using adrenaline auto-injectors.
- Children to receive advice from allergy dieticians, to ensure adequate nutrition (especially with the avoidance of nutritious food such as cow's milk, egg and wheat) and optimal growth.
Food oral immunotherapy (OIT) (also known as desensitisation) is a treatment option to improve the tolerance and quality of life in children with food allergies. Such therapy should only be initiated and guided by a paediatric allergist experienced in OIT.
- These children will consume the allergenic food daily, with the aim of gradually ingesting larger amounts without a reaction over time.
- Reactions to the food may still occur during the therapy. As such, it should only be initiated and guided by an experienced paediatric allergist, and dose increments conducted only in a controlled setting (such as a hospital or clinic equipped to handle allergic reactions).
- Symptoms can still occur when the child stops taking the allergenic food regularly, as oral immunotherapy is not a cure for the food allergy.
Refer a patient
Community health professionals can refer a child suspected with food allergies for assessment by the
KKH Allergy Service via KKH Central Appointments at
+65 6294 4050 or [email protected].
|
Food Allergy Awareness Roadshow 2025
|
Food allergy resources for parents and caregivers
References
- Goh, S. H., Yap, G. C., Cheng, H. Y., et al. (2024). Trends in Childhood Anaphylaxis in Singapore: 2015–2022. Clinical & Experimental Allergy, 54(8), 585-595.
- Cardona, V., Ansotegui, I. J., Ebisawa, M., et al. (2020). World allergy organization anaphylaxis guidance 2020. World allergy organization journal, 13(10), 100472.
|

|
Dr Chong Kok Wee, Head and Senior Consultant, Allergy Service, KKH
Dr Chong specialises in paediatric allergy, with research interests focused on food and drug allergies in children, oral immunotherapy and allergy prevention.
A strong advocate for patients and families dealing with food allergies, he co-authored a children's picture book titled "Milly and the Milk Disaster" as part of the
Baby Bear Paediatric Care Series, which he leads.
He also spearheads Project SAFE (Singapore Allergy Awareness for Everyone), a multi-agency patient advocacy initiative that encompasses food allergy awareness roadshows, EpiPen training workshops for primary and preschool teachers, development of food allergy resources for parents, and programmes to enhance food allergen safety among food service workers.
|
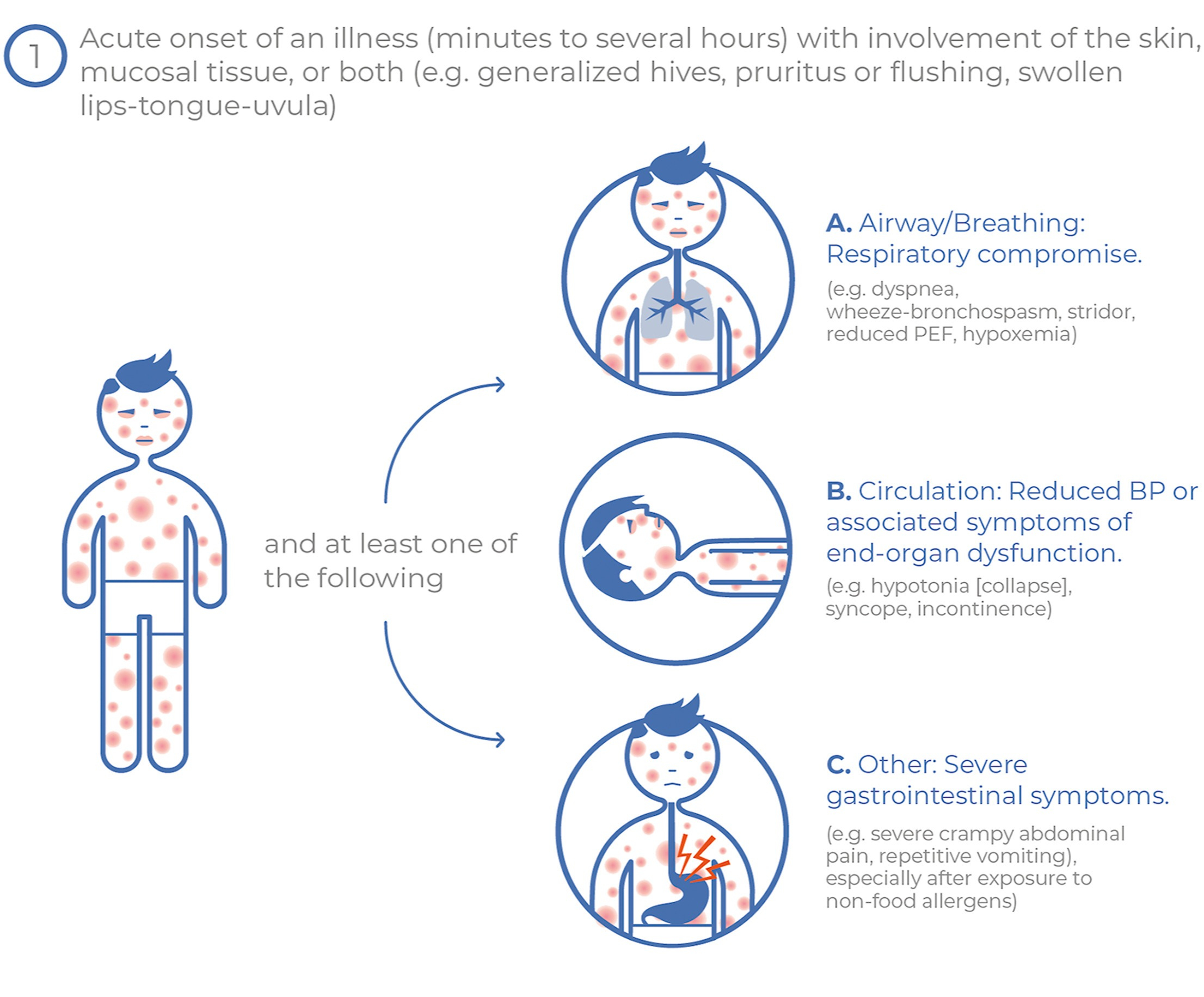
Annex A. World Allergy Organization (WAO) Diagnostic Criteria for Anaphylaxis (2020)2
Anaphylaxis is highly likely when any
one of the following two criteria are fulfilled:
|
1. Acute onset of an illness (minutes to several hours) with simultaneous involvement of the skin, mucosal tissue, or both (e.g. generalised hives, pruritus or flushing, swollen lips-tongue-uvula)
AND AT LEAST ONE OF THE FOLLOWING:
- Respiratory compromise (e.g. dyspnoea, wheeze-bronchospasm, stridor, reduced PEF, hypoxemia)
- Reduced blood pressure or associated symptoms of end-organ dysfunction (e.g. hypotonia [collapse], syncope, incontinence)
- Severe gastrointestinal symptoms (e.g. severe crampy abdominal pain, repetitive vomiting), especially after exposure to non-food allergens
|
Source: World Allergy Organization |
OR
|
2. Acute onset of hypotension or bronchospasm or laryngeal involvement after exposure to a known or highly probable allergen for that patient (minutes to several hours), even in the absence of typical skin involvement.
| 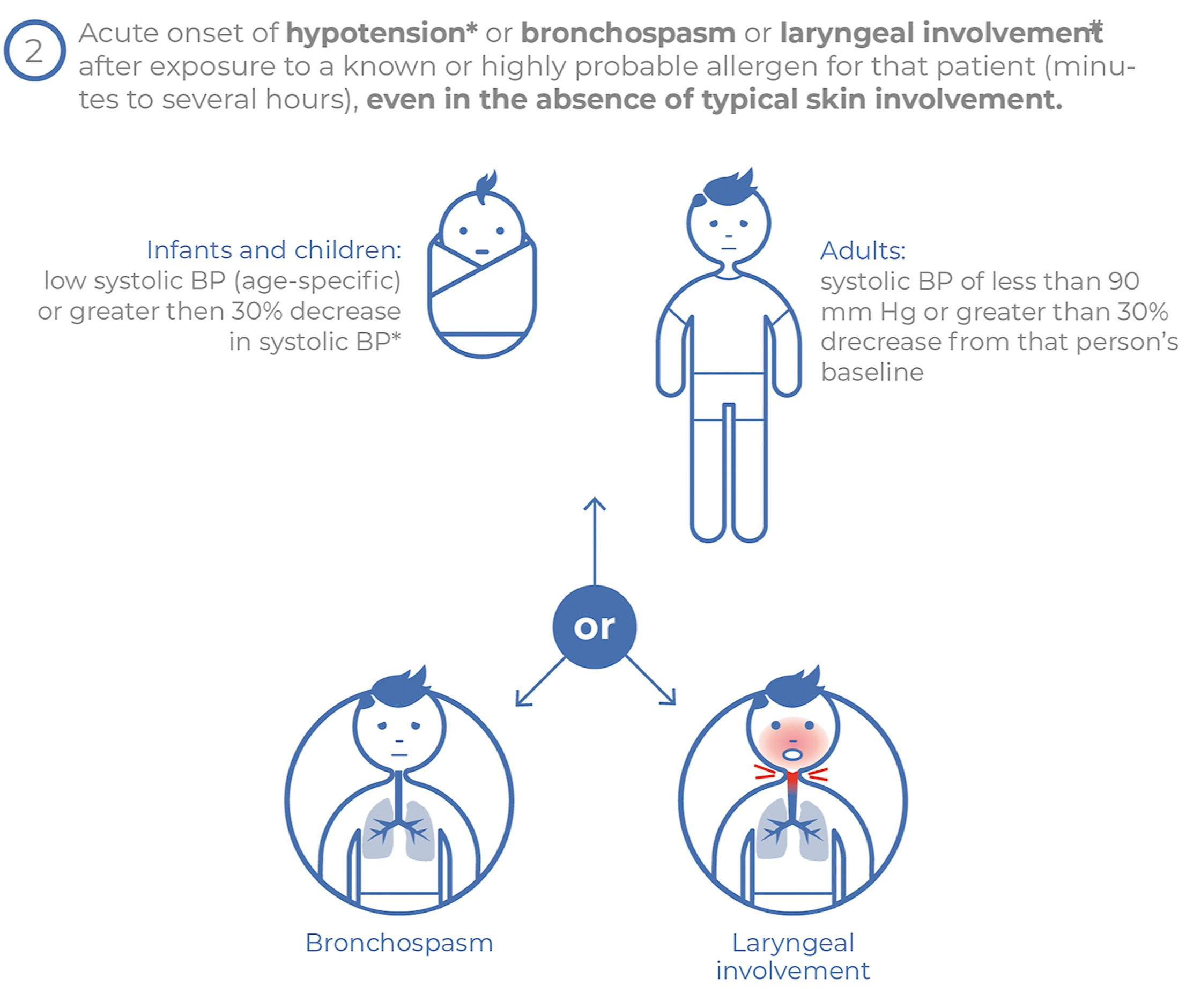
Source: World Allergy Organization
|
Annex B. KKH Allergy Action Plan
