Many asthma patients can be managed effectively in the primary setting with interventions such as appropriate emergency treatment and the optimisation of long-term management with regular review. The SingHealth Duke-NUS Lung Centre shares more.
Although Singaporeans have access to one of the most advanced healthcare in the world, preventable asthma deaths still continue to occur today because of excessive patient reliance on short-acting beta-agonists. Many of these patients can be managed effectively, however, in the primary setting with interventions such as appropriate emergency treatment to treat asthma exacerbations and trigger points, as well as the optimisation of long-term management with regular review.
INTRODUCTION
Asthma is a chronic condition with variable respiratory symptoms such as wheeze, breathlessness, chest tightness and cough characterised by chronic airway inflammation. It is one of the most frequently encountered chronic diseases in primary care clinics affecting around 5% of Singapore residents aged 18-69 years.1
Undertreatment of asthma, even in relatively asymptomatic patients, can lead to severe exacerbations resulting in hospitalisation or mortality. Such events, however, are preventable and the goals of good symptom control and reduction of exacerbation risk can be achieved in most patients with quality and holistic asthma care.
ASTHMA MORTALITY AND MORBIDITY REMAINS HIGH IN SINGAPORE TODAY
Despite the advances in asthma treatment over the past decade, Singapore’s asthma mortality and hospitalisation rates have continued to stagnate at levels that remain two to three times higher than other developed countries such as the United States and Japan.
In a survey of eight Asia-Pacific countries, one in two asthmatics in Singapore reported missing school or work while one in three asthmatics reported having an exacerbation in the preceding year.2 In the same study, it was also found that Singapore ranked lowest in the usage of preventer medications with only one in four asthmatics reporting usage in the previous month.
Although there have been advancements in the accessibility to healthcare and treatment options for asthma in Singapore, significant quality gaps in asthma care remain that contribute towards asthma mortality and morbidity. An audit of 340 patients hospitalised for fatal and near-fatal asthma in four restructured hospitals in Singapore from 2011-2015 was performed, and it found that 17.1% had no regular asthma follow-up and 32.1% were not on any inhaled corticosteroids (ICS).3
It is imperative that we close these gaps in quality if we are to achieve further reductions in mortality and morbidity.
CLINICAL VIGNETTE
Mr C, a 30-year-old man, presents to your clinic with shortness of breath and chest tightness for a 3-day duration. He is an active smoker and has a history of asthma since childhood.
He relies on his salbutamol inhaler for symptom relief up to four times daily, even though he was previously prescribed an ICS inhaler. He only sees his general practitioner (GP) three to four times a year for nebulisations and when he is unable to relieve his symptoms with his salbutamol inhaler.
Many GPs have encountered patients like Mr C who only seek episodic and unscheduled emergency care for asthma. How can we improve the quality of their asthma care in Singapore?
WHAT INTERVENTIONS CAN IMPROVE THE QUALITY OF MR C’S ASTHMA CARE?
1. Effective emergency medical treatment of asthma exacerbations, addressing trigger factors, and initiation of appropriate long-term management with early outpatient medical review
Oral corticosteroids
Patients who present for acute asthma exacerbations like Mr C should be treated with a 5-7 day course of oral corticosteroids (OCS) such as prednisolone (30–40 mg/day) within one hour of presentation, to speed up resolution of exacerbations and prevent relapse.
ICS-containing preventer
It is also recommended that patients be initiated on an ICS-containing preventer, if not previously prescribed. If the patient is already receiving an ICS-containing preventer, they should have their preventer treatment stepped up for 2-4 weeks. Inhaler technique should be demonstrated and checked.
Written asthma action plan
All patients should also be issued a written asthma action plan (WAAP). The WAAP should include details of the patient’s usual asthma medications, instructions on how to recognise worsening asthma and the necessary actions to take, which range from increasing the ICS dose or using OCS to seeking emergency help in addition to reliever use.4 Possible reasons for the exacerbations and appropriate advice should be given, such as smoking cessation and avoidance of common triggers (exposure to allergens, irritants, pollution, drugs, etc.).
Early outpatient medical review
Finally, an outpatient follow-up appointment within 1-2 weeks should be issued to their usual healthcare provider to review the patient’s symptoms and ensure that asthma treatment is continued.4
2. Optimising long-term management of asthma with ICS and regular medical review
Benefits of ICS over short-acting beta-agonist treatment
ICS reduces airway inflammation and is the most effective management option for asthma. It significantly reduces the risk of asthma exacerbation and mortality with benefits derived at low doses even in patients with infrequent asthma symptoms. ICS also improves lung function, asthma symptoms and control, and reduces missed days at work or school as well as healthcare costs.4,5
Although short-acting beta-agonist (SABA) treatment is effective for quick relief of asthma symptoms, it does not address the underlying pathology of chronic airway inflammation. In fact, overuse of SABA is associated with increased risk of death and exacerbation.
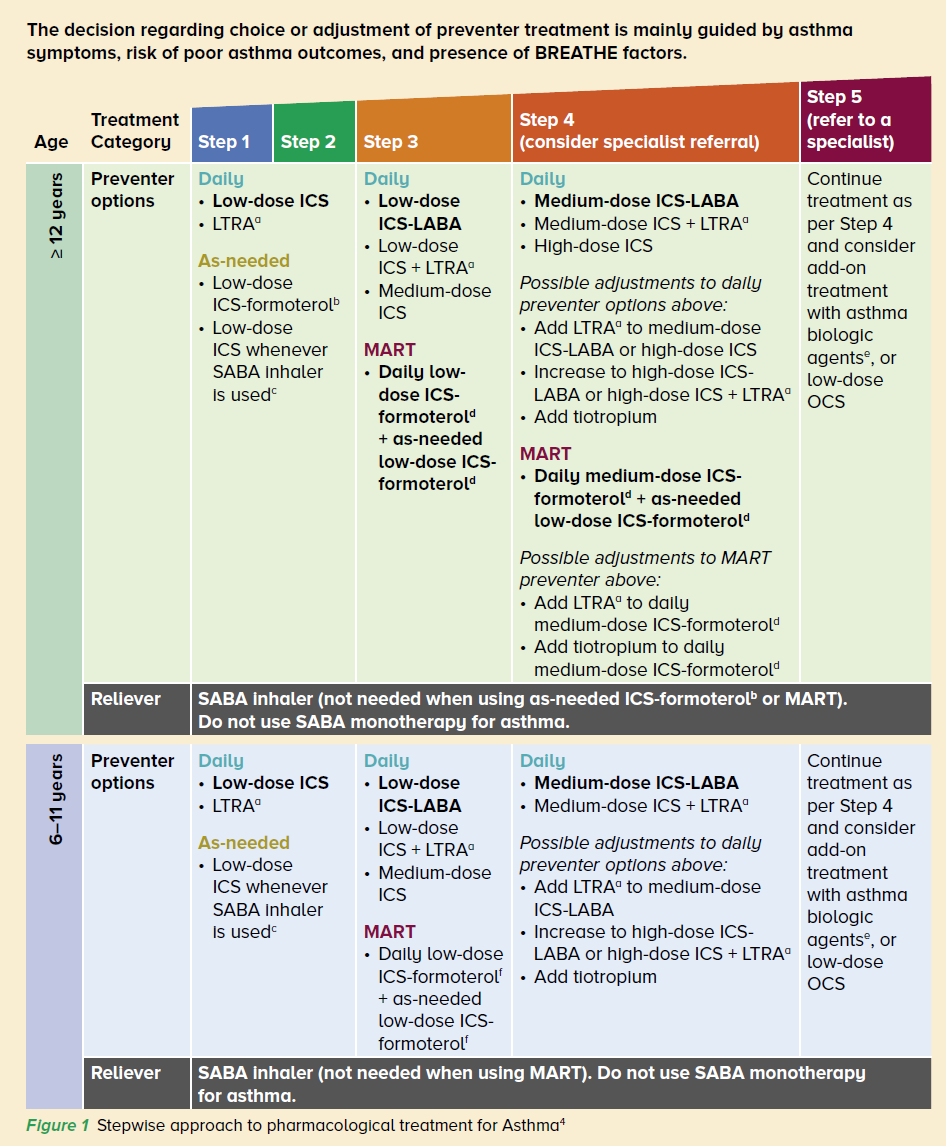
Based on evidence from clinical trials and real world data, Singapore’s Ministry of Health Agency for Care Effectiveness (ACE) Clinical Guidance for Asthma (2020) recommended ICS as the mainstay of long-term asthma treatment for step 1 (for all ages) (Figure 1).
The use of SABA alone (without a preventer) is no longer recommended for the long-term treatment of patients aged 6 years and older, even those with infrequent or minor symptoms.4 This was also reflected in the Global Initiative for Asthma (GINA) strategy report which was revised significantly in 2019 to recommend the prescription of (1) as-needed
budesonide-formoterol or (2) as-needed ICS whenever SABA is taken, for step 1 treatment instead of SABA PRN.5
Regular medical review
After initiation of ICS-containing preventer medications, patients like Mr C should be regularly reviewed at least twice yearly to assess their asthma control with validated questionnaires such as the Asthma Control Questionnaire (ACQ), the Asthma Control Test (ACT) or other validated questionnaires.4
A patient with well-controlled asthma should have no symptoms and no exacerbations. Consideration should be given towards treatment escalation in stepwise fashion (Figure 1) if patients continue to have frequent or intensive symptoms, especially if risk factors for severe asthma outcomes are present (Figure 2).
3. Timely referral to a respiratory specialist for difficult-to-treat asthma
Although most patients with asthma can be managed effectively in primary care, GPs should consider specialist referral if:
- The diagnosis of asthma is uncertain, for further diagnostic evaluation with lung function tests like spirometry and bronchial provocation testing,
- Patients continue to have persistent or worsening symptoms despite stepping up of preventer treatment,
- Patients require medium-to-high doses of ICS-containing treatment or long-term oral corticosteroid therapy (patients on step 4 or 5 treatment), for consideration of biologic therapy;
- Or for specific subgroups of patients with asthma such as pregnant patients, patients with occupational asthma, elderly patients, or athletes.
RISK FACTORS FOR SEVERE ASTHMA EXACERBATIONS OR MORTALITY- SABA monotherapy or usage of ≥ 1 canister of salbutamol in ≤ 2 months
- Suboptimal ICS use
- History of intubation or admission to ICU for asthma
- History of one or more exacerbations in the past year
- Cigarette smoking (past or present)
|
In summary, Mr C’s asthma care can be optimised by:
- Treating his current asthma exacerbation with a course of prednisolone 30 mg daily for 5 days and addressing possible trigger factors
- Initiating an ICS-containing long-term treatment for him
- Giving him an outpatient appointment in 1-2 weeks to review his response to treatment for exacerbation, and regular follow-up for asthma at least twice yearly thereafter
- Providing asthma education, inhaler technique training and issuing a personalised WAAP to optimise self-management
- Advising him to quit smoking and receive vaccinations for influenza and pneumococcal disease as per the National Adult Immunisation Schedule in Singapore
- Considering him for specialist referral if his asthma symptoms remain uncontrolled or he continues to have exacerbations
THE SGH SEVERE/DIFFICULT-TO-TREAT ASTHMA CLINICThe SGH Severe/Difficult-to-Treat Asthma Clinic was set up in 2011 and provides highly specialised care for patients with difficult-to-treat or severe asthma. It comprises of a multidisciplinary team of respiratory specialists, asthma nurses, pharmacists and physiotherapists with the goal of helping asthma patients achieve optimal asthma control. We offer specialised tests to aid in diagnosis and phenotyping of asthma (e.g., induced sputum). Advanced treatments such as biologics (anti-IgE, anti-IL5/IL5R) as well as bronchial thermoplasty are also available. In addition, patients also have options to participate in clinical trials and research. HOW GPS CAN REFER
To refer a patient to the SGH Severe/Difficult-to-Treat Asthma Clinic, GPs can contact the Clinic at: Tel: 6326 5361
Email: [email protected] For more information on the Clinic, visit the website. |
REFERENCES
- Epidemiology and Disease Control Division MoH, Singapore. National Health Survey. 2010. Available at: www.moh.gov.sg/resources-statistics/reports/national-health-survey-2010. Accessed 22 April 2020.
- Thompson PJ, Salvi S, Lin J, et al. Insights, attitudes and perceptions about asthma and its treatment: findings from a multinational survey of patients from 8 Asia-Pacific countries and Hong Kong. Respirology (Carlton, Vic). 2013;18(6):957-67
- Yii ACA, Puah SH, Lim HF, et al. A national audit of severe life-threatening asthma in Singapore. European Respiratory Journal Sep 2018, 52 (suppl 62) PA3957
- Agency for Care Effectiveness, Ministry of Health Singapore. Clinical Guidance - Asthma: Optimising long-term management with inhaled corticosteroid. 2020 Oct 1. Assessed 04 January 2021 at https://www.ace-hta.gov.sg/our-guidance/asthma%E2%80%93optimising-long-termmanagement-with-inhaled-corticosteroid.html.
- 2020 GINA Report, Global Strategy for Asthma Management and Prevention. Assessed 04 January 2021 at https://ginasthma.org/wp-content/uploads/2020/06/GINA-2020-report_20_06_04-1-wms.pdf.
Dr Chew Si Yuan is an Associate Consultant in the Department of Respiratory & Critical Care Medicine, Singapore General Hospital. He graduated from the National University of Singapore and completed his Respiratory Medicine and Intensive Care Medicine training in Singapore. He has a keen interest in medical education and is active in teaching medical undergraduates and residents from both internal medicine and family medicine.
GPs who would like more information about this service, please contact Dr Chew at [email protected].
GPs can call the SingHealth Duke-NUS Lung Centre for appointments at the following hotlines, or scan the QR code for more information:
Singapore General Hospital: 6326 6060
Changi General Hospital: 6788 3003
Sengkang General Hospital: 6930 6000
KK Women’s and Children’s Hospital: 6692 2984
National Cancer Centre Singapore: 6436 8288
