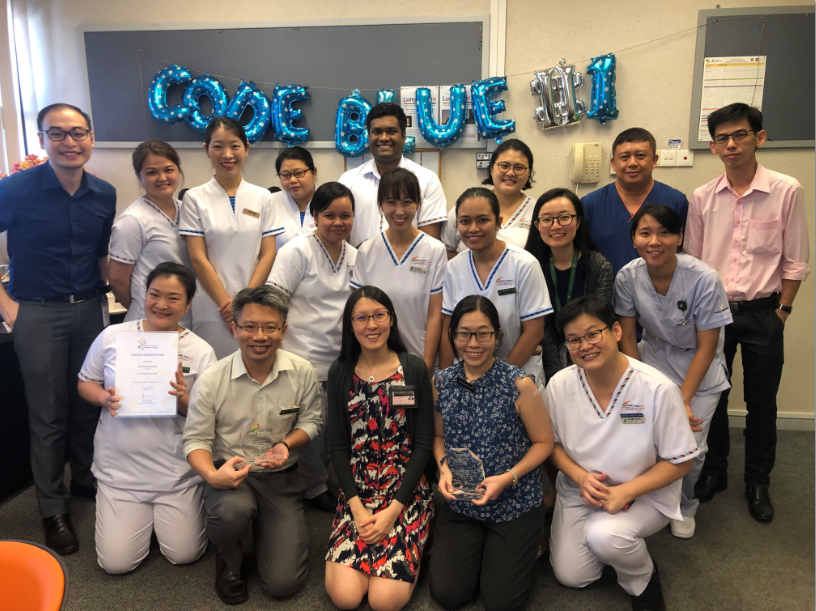
For their effort, the team led by Dr Carrie and Dr Claudia won the Quality Improvement Project of the Year at the recent SGH Quality Convention, as well as numerous awards such as the SingHealth Family Target Zero Harm Award and SGH Innovation & Quality Circle Star Award.
Embarking on a redesign of processes on an organizational scale – especially a matrix organization like SGH - is a monumental task. Yet the Code Blue team did it in just 6 months. At the centre of their success is their ability to get myriad stakeholders across staff groups, departments and even institutions onboard their change initiative. Lighternotes spoke to the team to find out how they achieved buy-in.
Every month, SGH gets about 22 Code Blue calls. When a patient stops breathing, or when his heart stops beating, his chance of survival drops by 10 % with every passing minute. So it is critical that he be resuscitated as soon as possible.
A 2017 Joint Commission International (JCI) audit showed that our average Code Blue response time from 2015 to 2017 was slower than the 5-minute JCI benchmark. The audit also found that improvements could be made to our manpower, skills set and equipment for code blue response.
SGH Medical Board tasked a multi-disciplinary team led by Dr Carrie Leong, Consultant, SGH Respiratory & Critical Care Medicine, and Dr Claudia Tien, Consultant, SGH Surgical Intensive Care, to redesign the process of response. The team managed to speed up SGH’s code blue response time to less than 5 minutes within a mere six months. This response time is no mean feat considering that SGH has 1,700 beds spanning six blocks.
Previously, the Code Blue response was discipline-based and by a single doctor. With the revamp, the Code Blue Team nearest to that patient is activated. This team is also multi-disciplinary (doctor, nurse, Respiratory Therapist) and specialise in resuscitative skills and equipment. Explained Dr Carrie, “Code Blue is a medical emergency. Hence, it requires a specialised team trained in resuscitative skills and equipment for efficient and effective patient care.”
The team shared how they managed to redesign processes to deliver faster and more effective care.
1. Find common ground
“Our stakeholders had competing priorities. So it was difficult to bring everyone together for this initiative. We had to find common ground to get buy-in,” shared Dr Claudia, “We collected data and used that to convince our stakeholders that we were all facing the same problems. Coupled with our shared passion for improving patient care, our stakeholders came onboard.”
2. You don't have to go it alone
Dr Tan Hui Li, Nurse Clinician (APN), said that the new code blue team required additional manpower and involvement from different staff. “Previously, only doctors responded to a Code Blue,” she explained, “and we wanted to boost the capabilities for effective resuscitation and provide 24/7 coverage. Thus we sought partnerships from all the ICUs and developed rosters. We even got nurses from National Heart Centre to provide coverage for SGH Block 4! Top-down support from SGH and NHCS Chief Nurses and nursing administrators helped us get the resources and manpower. Also prior to this project, we had already built a spirit of collaboration among all ICUs through routine interactions, multi-ICU training programmes and Quality Improvement projects. We also engaged staff via multiple dialogues to address their concerns and anxiety. And we followed through with comprehensive training. So the ICUs and NHCS nursing readily supported the Code Blue team when we asked for help.
3. Do your ground work
A lot of effort was spent brainstorming, collecting data and doing background research,” shared Dr Claudia, “I remember walking around SGH for 5 hours one afternoon to identify and name all the various locations within SGH so that we could develop a common directory of locations for Call Centre to refer to when they received a call! Establishing a common directory of locations allows those who activate the Code and Call Centre to speak the "same language" so that essential information (i.e. the location) is not lost in translation. In an emergency, it is natural that people will panic and struggle to identify the location of the arrest, resulting in miscommunication and frustration for all. I think it is important to go down to Call Centre and also to each of the many locations within SGH so as to put myself in the shoes of those using the system in order to create a better system together.”
4. Practice, practice, practice!
A rapid and robust Code Blue response is about delivering the right care, right now. Explained Dr Carrie, “Our Code Blue teams comprising Registrars, Respiratory Therapists and ICU-trained nurses undergo annual simulation trainings together. This way, team members become familiar with each other’s roles and are able to anticipate tasks without prompting – this makes for a more rapid and effective resuscitation effort.”
.png)
Team members undergo regular simulation training together so that they can function like a well-oiled Formula 1 pit-stop crew to deliver life-saving interventions rapidly.
Rigorous trainings and simulations were also conducted for the call centre staff on the Code Blue team to be familiarised with the revised Code Blue workflow prior to roll-out,” said Ms Hong Xiaowen, Senior Operations Executive, Call Centre & Telecommunications.
5. Celebrate small successes
“It is important to celebrate small successes and share them with the entire team, so that people feel motivated to go on for the long haul,” Dr Claudia explained, “It can be exciting at the start but people can lose steam because the hospital is a busy place.”
6. Seek first to understand
Ms Xiaowen shared, “Each department has their own operational workflow and reasons for doing things, it is crucial to fully understand the current process of all parties involved before forming a solution. Otherwise – instead of solving the problem - the proposed solution may create even more issues.”

SGH Quality Convention 2020 Project of the Year Award Ceremony
We love mail! Drop us a note at lighternotes@sgh.com.sg to tell us what you like or didn’t like about this story, and what you would like to see more of in LighterNotes.













 Get it on Google Play
Get it on Google Play