Deep vein thrombosis (DVT) used to be nicknamed the “economy-class syndrome” but DVT doesn’t occur to just those travelling on planes.
What is deep vein thrombosis (DVT) and why can it be dangerous?
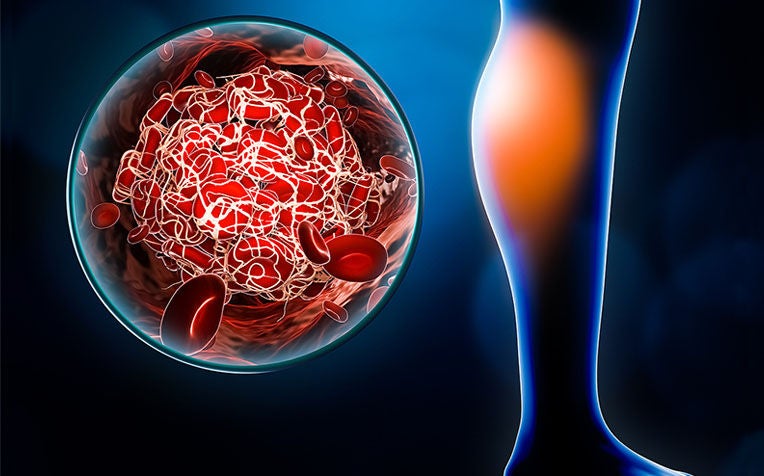
Deep vein thrombosis (DVT) is a blood clot (also called a thrombus) that forms in a vein deep in the body. Most deep vein clots occur in the leg or thigh but can also occur in other parts of the body.
This clot may interfere with circulation and it may break off and travel through the blood stream and lodge in the lungs, causing severe damage to that organ. If the clot lodges in the lung, it is called pulmonary embolism (PE).
"Pulmonary embolism (PE) is a very serious condition that can cause death. DVT and PE are collectively called venous thromboembolism (VTE) and are predisposed by the same risk factors," explains doctors from the Department of General Surgery from Singapore General Hospital (SGH), a member of the SingHealth group.
Deep vein thrombosis (DVT): How to prevent
There are ways to prevent this silent killer from striking.
Keep moving: Don’t sit in a cramped position for too long. Wriggle your toes and work those ankles and knees. Make an effort to stand up and walk \to get the blood pumping. When embarking on long haul flights, ask for an aisle seat if possible. Studies have shown that passengers in window seats have double the risk of developing DVT.
Sit right, not tight: Don’t cross your legs or sit on the edge of the seat. Wear loose clothing, and avoid stockings or socks with tight bands.
Avoid alcohol and caffeine when flying: Don’t let yourself be intoxicated or dehydrated before and during a long-haul flight. Instead, drink water at regular intervals.
Avoid taking sleeping pills when on a flight: This encourages immobility and increases the risk of DVT.
Wear travel compression socks: These are designed to encourage the upward flow of venous blood in the lower limbs, thus preventing the pooling of blood in the veins and reducing the risk of blood clotting.
Always consult your doctor if you have any health concerns with regards to air travel. This is especially true if you have an existing health condition that may increase your risk of DVT.
Your doctor will be able to assess your probability of developing DVT based on your medical history and current condition.
Deep vein thrombosis (DVT): Risk factors
Even the healthiest souls among us can succumb to DVT, but the following are especially at risk.
Prolonged sitting, such as passengers on long flights or drives. Also, prolonged bed rest, especially for people with paralysis or those hospitalised for a long period of time, are risk factors for DVT. When your legs remain still for many hours, the muscles of the legs do not contract. Muscle contraction is important for good blood circulation, and absence of contraction can cause blood clots to form in the legs.
Although DVT can develop at any age, people aged 60 and above are at higher risk of DVT.
Those with inherited blood clotting conditions. If someone in your family has a history of DVT, you may have a higher risk for developing the same condition.
Pregnant or post-partum women. This is because pregnant women have high pressure in the veins of the pelvis and the legs which increases the risk for blood clots to form.
Those who are overweight or obese as they have higher pressure in the veins of the pelvis and the legs.
People with severe varicose veins may be more likely to develop DVT.
Certain types of cancer and some forms of cancer treatment increase the risk for DVT.
Any type of injury to a vein, such as when surgery is performed or when there is trauma, can increase the risk for blood to clot in the affected vein.
Those taking contraceptive pills or who undergo hormone therapy have a greater risk for DVT.
Deep Vein Thrombosis (DVT): Symptoms to watch for
Those suffering from deep vein thrombosis (DVT) usually feel muscle pain, tenderness, swelling and redness around the calves of the leg.
In severe cases, the swelling can extend up to the thigh and hip level. Sometimes, it can take up to two weeks for the symptoms to become apparent.
But DVT is only potentially life-threatening when the blood clot breaks away from the vein and lodges itself in the lungs. When the clot blocks the flow of blood to the heart, a condition known as pulmonary embolism (PE) develops. In the most severe cases, PE could lead to collapse, a drop in blood pressure and sudden death.
It is only in recent years that deep vein thrombosis has gained notoriety. And this came after headline reports of long-haul flight passengers collapsing after hours spent confined in tight seats.
Although the condition was nicknamed the “economy-class syndrome”, DVT doesn’t just occur to those travelling on planes.
Deep vein thrombosis (DVT): How to manage
The cornerstone in the treatment of deep vein thrombosis (DVT) is the use of medications called anticoagulants or "blood thinners".
Such medications slow down the formation of blood clots to allow the body's natural system to remove the clots and reduce the recurrence of DVT.
The anticoagulation medications include injectables such as heparin or low molecular weight heparin, or tablets to be taken orally, such as apixaban, dabigatran, rivaroxaban and warfarin.
The main complication of treatment with anticoagulation medications is bleeding. It is important to have regular follow up consultations and necessary blood tests to prevent and reduce the bleeding risks.
Ref: I23 (ed)
Check out other related articles:
Flying Risks and Prevention Tips















 Get it on Google Play
Get it on Google Play