The making of ocular prostheses involves the work of prosthodontists who specialise in restorative dentistry.
The making of glass eyes began as early as the 16th century in Venice, Italy, while other forms of artificial eyes were introduced even before that. The art of ocularistry, a niche field of making prosthetic eyes, and its links to dentistry, can be traced back to 1943, when dental technicians in the United States Army created the first impression-fitted acrylic eyes using dental materials. Until today, prosthetic eyes are mostly made of acrylic.
Indeed, there are many commonalities between ocular and dental prosthetics. In SingHealth, the prosthetic eye fitting service, a highly specialised treatment that requires the combined effort of an ophthalmologist and a maxillofacial prosthodontist, is offered at Singapore National Eye Centre (SNEC), in collaboration with the National Dental Centre Singapore (NDCS).
Coordinated care
The Ocular Prosthetic Clinic, led by Clinical Associate Professor Teoh Khim Hean, Senior Consultant at NDCS’s Prosthodontic Unit, was established in 2003 as part of SNEC’s drive towards patientcentric care.
Prof Teoh, who is also Deputy Director for Clinical and Regional Health at NDCS, specialises in Prosthodontics, which involves procedures such as restoration of teeth, maxillofacial prosthetics, and implant rehabilitation.
“The overall management and treatment of a patient who loses one or both eyes are highly complex, and require a multidisciplinary approach to achieve the best possible outcome. We wanted to offer a convenient one-stop centre for patients who require ocular prostheses, and saw real value in creating a seamless integrated pathway for patients to receive such care in one setting. With the collaboration, we can harness our collective expertise and work closely with ocular plastic surgeons in SNEC to improve patients’ lives,” said Prof Teoh.
This highly coordinated care is evident in NDCS too. Laboratory skills honed in dentistry are also essential in the making of ocular prostheses. “The concept and process of fabricating ocular prostheses for eye sockets are similar to that of making dentures for the mouth,” added Prof Teoh, who also trains junior prosthodontists and lab technicians in fabricating ocular prostheses.
A boost of confidence
For most patients, the loss of an eye is a traumatic experience that has devastating psychosocial consequences. Often, these patients feel conscious about their appearance. Having a prosthetic eye can help them regain confidence, restore essential daily functions, and ultimately improve their quality of life.
Fun fact
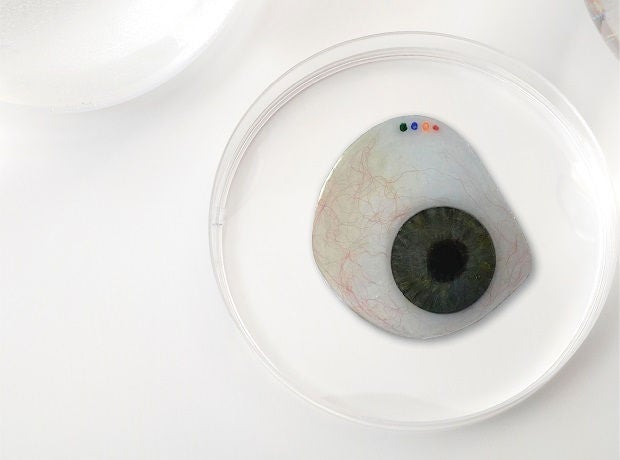
The veins in the sclera (white part of the eye) of the prosthetic eye are made using red silk threads.
In some severe cases, a patient may have lost an eye due to the extension of a tumour from the mouth to the eye socket. This would have resulted in the removal of the upper jaw, eyeball and eyelids, and would affect speech, swallowing and appearance.
In such situations, an obturator and an orbital prosthesis are created to fill the spaces in the oral (mouth) and orbital (eye) cavities respectively. For these patients, having a maxillofacial prosthesis can help restore the function of swallowing and make eating a more comfortable experience. It also helps with speech pronunciation to improve communication.
What to expect
The making of prosthetic eyes is as much an art as it is a science. Every piece is customised to meet the needs of each patient.
The process begins six weeks after the surgical removal of the eye. An impression tray is inserted into the ocular cavity and a mould is taken to determine the size of the prosthesis.
The iris is designed and matched with the patient’s other eye, or with a photograph of the original eye. “The challenging part comes when there are variations and shades of brown or black that require careful curation of colours to create a realistic look,” said Prof Teoh. “Currently, we are also exploring 3D-printing technology to make the fabrication process more efficient. This potentially offers significant time savings.”
Once completed, the prosthesis is then inserted where it can move like a normal eye.
“Patients are inevitably worried about changes and their ability to adapt. Very often, I get questions about how to wear the prosthesis, whether it will fall out, the types of activities that can or cannot be done, and how the prosthesis will look like when worn,” said Prof Teoh. “I educate them on the use, maintenance and management.”
The prosthesis can be worn for the entire day and removed for cleaning when there is discharge. Annual polishing is encouraged to remove any build-up of discharge and ensure that the prosthesis is kept in good condition.
Did you know?
Patients who have lost one eye suffer from 25 per cent reduction of vision. Their binocular vision is also halved.













 Get it on Google Play
Get it on Google Play