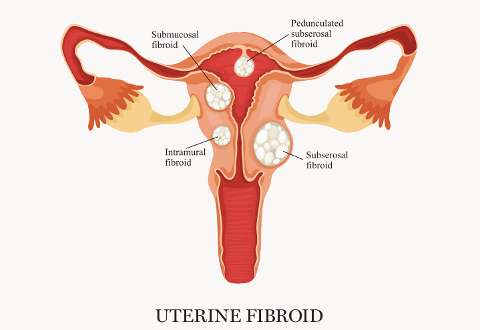
Uterine fibroids (also known as leiomyomas or myomas) are the most common pelvic tumours in women, affecting one in five women during their reproductive years. While the prevalence increases with age during the reproductive years, these benign tumours only rarely develop into cancer.
Patients typically present with one or more symptoms such as abnormal uterine bleeding (heavy, prolonged or painful menstrual bleeding) and pelvic pain, or pressure-related symptoms that can interfere with their lifestyles.
Large uterine fibroids can compress surrounding pelvic structures, causing urinary frequency, constipation and abdominal bloating. More uncommonly, they may cause dyspareunia and reproductive dysfunction, such as infertility or adverse pregnancy outcomes.
The exact aetiology of uterine fibroids is unknown, although oestrogen stimulation is involved and uterine fibroids are known to grow rapidly in pregnancy but stop growing and shrink after menopause.
Asymptomatic fibroids may be followed without intervention. For symptomatic patients, medical therapy, in the form of hormonal drugs (such as progesterone or gonadotropin-releasing hormone) may provide adequate symptomatic relief from pain and abnormal bleeding for some women.
When medical therapy fails or symptoms are debilitating, fertility-sparing myomectomy – surgery to remove the fibroid while leaving the uterus intact – has traditionally been the standard treatment option.
A major surgery requiring up to six weeks for full recovery, myomectomy may be performed by various techniques and is associated with a 10 to 25 percent risk of fibroid recurrence. Patients who have completed their families may be offered total hysterectomy.
Uterine artery embolisation
Uterine artery embolisation is a minimally invasive treatment option that has matured over the past 20 years, offering select patients with uterine fibroids an alternative to surgical intervention. It can also be performed as part of a staged procedure to reduce the size of the uterus prior to hysterectomy.
Compared to surgical intervention, patients undergoing uterine artery embolisation can expect to experience a shorter duration of hospitalisation, faster recovery and lower morbidity risk. The procedure is also a particularly attractive option for those who present with prolonged heavy and/or painful menstrual bleeding, but are averse to or unfit for surgery.
Most patients (73-90%) report improvement or relief of heavy menstrual bleeding up to 10 years after treatment. Patients who are eligible for uterine artery embolisation include those who do not have current or recent pelvic infection, are not pregnant and have no desire for future pregnancy.
At KK Women’s and Children’s Hospital (KKH), uterine artery embolisation is performed by the interventional radiologist for patients with symptomatic fibroids. A small (< 5mm) skin incision is made at the groin region for access to the femoral artery. Using fluoroscopy, the radiologist manipulates a guide wire and catheter to the uterine arteries supplying the fibroid.
Nanometre embolic particles are injected selectively into these arteries (Figure 4) to occlude the blood flow and induce fibroid ischaemia, necrosis and shrinkage. Light sedation is usually administered during the procedure in addition to patient-controlled analgesia.

After the procedure, oral analgesics are prescribed for pain management, and the majority of patients are usually discharged within one or two days. Patients will be reviewed regularly to monitor for post procedural effects, such as post embolisation syndrome – which can present as self-limiting fever, nausea, pain and malaise within the 10 to 14 days after the procedure.
Vaginal discharge is also relatively common (in 16-20% of patients) and can persist for up to 12 months, though it is usually self-limiting, non-purulent and not associated with fever. Supportive management is usually adequate to manage these.
Fibroid shrinkage is an expected and desirable outcome of uterine artery embolisation; another possible desirable outcome is fibroid expulsion that may be accompanied by pain similar to labour pains.
Recurrence of severe pain after a pain-free period may indicate impending fibroid expulsion; pain coupled with foul-smelling purulent discharge indicates infection. Patients presenting with these symptoms are recommended to seek prompt review and assessment at the Women's 24-hour Clinic* at KKH, so that appropriate treatment can be administered.
After three months, patients will be assessed to determine the results of uterine artery embolisation, such as a reduction in menstrual flow, symptoms related to mass effect, and to monitor for any remaining post embolisation syndrome. Patients will also undergo ultrasound after six months and magnetic resonance imaging after one year to provide continual assessment of symptoms and determine the size and extent of any residual fibroids.
Four to five patients undergo the procedure at KKH each year, with excellent technical and clinical success reported. Patients who had formerly experienced heavy menstrual flow have reported reduced flow, significant shrinkage of fibroids and even complete resolution in some cases.
A small proportion of patients (10-15%) may experience persistence of symptoms such as menorrhagia and anaemia, or recurrence of symptoms within four to five years, necessitating repeat embolisation. Subsequent hysterectomy may also be required in the case of refractory uterine fibroid occurence, though this is rarely required.
Case study: Non-surgical resolution of uterine fibroids
In her mid-forties, JC presented with severe anaemia (haemoglobin level of 5.6g/dl) and multiple large fibroids (Figure 1), accompanied by bloatedness, cramps, constipation and urinary frequency.
She also experienced prolonged heavy menstruation lasting up to two weeks per cycle, which had progressively worsened over 10 years, and a history of multiple uterine fibroids even after undergoing a myomectomy more than a decade prior.
At KKH, she was given a blood transfusion and prescribed iron supplements, after which her haemoglobin level hovered between 7 and 9g/dl. As JC had multiple large fibroids, she was recommended to undergo a uterine artery embolisation to reduce the size of the fibroids, with the intent to follow with a hysterectomy. After undergoing the embolisation procedure, JC was reviewed regularly to monitor for post procedural effects.
Twelve days after the procedure, JC presented with fever and abdominal pain characteristic of post embolisation syndrome. Blood tests indicated elevation of her white blood cell count and inflammatory markers, and a computed tomography scan of her pelvis showed non-enhancement of the fibroids with areas of gas cavitation, suggestive of infarction (Figure 2).
She was admitted for treatment with intravenous antibiotics. After four days, the acute signs and symptoms abated, and she was discharged. Four weeks after discharge, JC reported a desirable outcome of the expulsion of a large fibroid and multiple smaller fibroids per vaginum. She was reviewed and found to be clinically well. While small fibroids remained (Figure 3), she experienced significant improvement to her menstrual cycle and flow, with no bloatedness, cramps, constipation or urinary frequency. She also no longer required a hysterectomy.

*From 2018, the Women’s 24-hour Clinic has been renamed the Urgent O&G Centre (UOGC).

| Dr Jasmine Chua, Senior Resident, Department of Diagnostic and Interventional Imaging, KK Women’s and Children’s Hospital Dr Jasmine Chua graduated from the Yong Loo Lin School of Medicine and is currently pursuing further training in vascular and interventional radiology under the SingHealth Diagnostic Radiology Residency Program. Dr Chua’s clinical interests include interventional radiology unique to children’s and women’s health. |
 | Fellowship trained in paediatric interventional radiology, Dr Luke Toh heads the interventional radiology service at KKH. He has a special interest in the management of vascular malformations and is actively involved in the management of fallopian tubal recanalisation, morbidly adherent placentae and embolisation for post-partum haemorrhage. As Director, Talent Management, SingHealth Radiological Sciences Academic Clinical Programme, Dr Toh oversees mentorship programmes for the development of young radiologists. He is also Adjunct Assistant Professor with Duke-NUS Medical School, Singapore. Dr Toh is also a visiting consultant with the Department of Diagnostic Radiology at Singapore General Hospital, and teaching faculty with the Singapore Medical Association’s Centre for Medical Ethics and Professionalism. |
References:
|
Contributed by

English
Non-Surgical approach to uterine fibroid management_Special Delivery Vol 66 Issue 2.pdf















 Get it on Google Play
Get it on Google Play