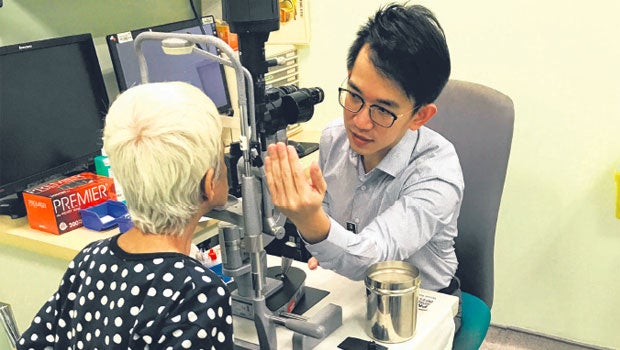
Dr Wong Chee Wai (left), a consultant at SNEC seen here examining a patient's eyes, said the new drug treatment is more effective as it selectively targets inflammatory cells within the eye. Professor Tina Wong (above) of the Singapore Eye Research Institute said it is a welcome alternative for doctors as it removes the problem of patients not complying with instructions to use eye drops.PHOTOS: SINGAPORE NATIONAL EYE CENTRE
Frequent application of steroid eye drops not needed with new method used by S'pore, Dutch researchers
Patients who have undergone cataract surgery have to apply steroid eye drops every three to four hours each day, for up to one month or longer, in order to control eye inflammation that occurs after the surgery.
But it is common for them to find eye drops difficult to apply, or to use them wrongly or forget to use them. And when eye inflammation is not controlled properly, it can lead to pain, blurred vision and in severe cases, even blindness.
Researchers at the Singapore National Eye Centre (SNEC) and Singapore Eye Research Institute (Seri), in collaboration with Utrecht University in the Netherlands, have worked together since 2014 to address this problem. They have developed a new treatment that removes the need for eye drops.
In this treatment, liposomal prednisolone, a steroid wrapped in layers of lipid nanoparticles, is applied onto the eye at the end of cataract surgery. The lipid layers make liposomal prednisolone more attractive to inflammatory cells, which are activated in response to surgery. The inflammatory cells then engulf the liposomal prednisolone, after which the steroid is released inside the cells to reduce inflammation.
In clinical trials, this drug treatment completely eliminated inflammation after surgery with no side effects, said Dr Wong Chee Wai, a consultant in the surgical retina department at SNEC and the principal investigator of the study.
Cataract is the clouding of the eye's lens, which can lead to vision problems including dim or blurry vision and reduced night vision. In cataract surgery, the cloudy lens is replaced with an artificial lens.
Most patients who get cataract surgery are aged 50 and above.
Professor Tina Wong, head of the ocular therapeutics and drug delivery group at Seri, and co-principal investigator for the study, said the new drug treatment is a welcome alternative for doctors as well, as it removes the problem of patients not complying with instructions to use eye drops.
"If you tell them to use these eye drops every three hours for one month... people will forget," said Prof Wong, who is also head of the glaucoma department at SNEC.
Dr Wong also said steroid eye drops have limited efficiency as less than 5 per cent of the drug actually reaches the site of inflammation. The drug can also be easily removed from the eye through tears or blinking, he said.
In comparison, the new drug treatment is more effective as it selectively targets inflammatory cells within the eye. The lipids around the drug also keep it from being dispersed before it reaches the inflammatory cells.
The team concluded the first round of clinical trials last year.
Housewife Eyok Raiyah Abubakar, 64, volunteered for the trials when she had cataract surgery on her right eye at the end of last year.
Compared with using eye drops after an earlier cataract surgery on her left eye, the new treatment was more convenient and comfortable, she said. "It was a good operation with no complications."













 Get it on Google Play
Get it on Google Play