The research team was able to classify the aggressive cancer into three distinct subtypes so as to encourage the development of novel treatments.
For the 200 angiosarcoma patients who walked through the doors of the National Cancer Centre Singapore in the last 20 years, their prognosis was typically bleak, with a five-year survival rate of less than 20 per cent.
However, a new study led by the centre’s researchers is set to improve these odds through a personalised-medicine approach.
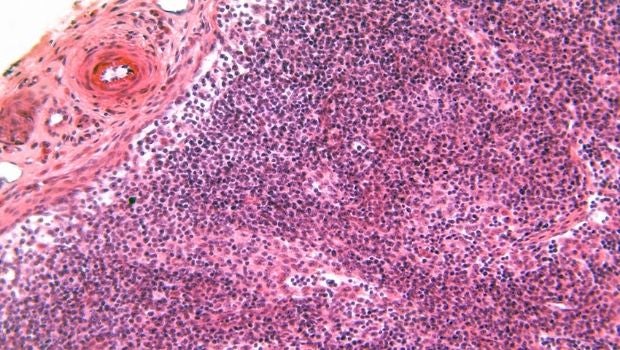
Angiosarcomas, clinically aggressive tumours found in the lining of blood and lymph vessels, can now be classified into three subtypes. These findings, published in The Journal of Clinical Investigation in October 2020, potentially unlocks targeted therapies and new treatments that can improve survival rates.
Angiosarcomas, while rare, are more prevalent among Asian populations, making up seven per cent of all sarcoma diagnoses in Asia. More than that however, the researchers noticed that “Asian-type” angiosarcomas tend to occur in the head and neck region of elderly men.
“This led us to speculate that there may be unique genetic or environmental factors influencing the manner of development of the disease,” said Clinical Assistant Professor Jason Chan, first author of the study and Consultant in the Division of Medical Oncology, NCCS.
Get updates on Tomorrow's Medicine in your mailbox! Click here to subscribe.
Understanding the unique signatures of angiosarcomas
Their investigation paid off. After studying the tumour samples of 68 patients at the NCCS and Singapore General Hospital between 2000 and 2015, the team found that angiosarcomas could be grouped into three distinct clusters based on various factors, such as the cause, which part of the body it’s found, risk factors, cell signaling pathways and the level of inflammation in the tumour.
NanoString profiling, a technology that profiles the expression of genes, revealed that patients in the third cluster had high inflammation and their cancer involved a significant defence response from the immune system.
Cluster one was similar to cluster three in that most of the tumours originated in the head and neck region, only with less inflammation. Meanwhile, patients in cluster two had angiosarcomas as a secondary cancer.
The scientists also found that 50 per cent of head and neck angiosarcomas was related to UV exposure and were highly mutated.
That’s not all. “Interestingly, we also observed that a particular virus known as Human Herpesvirus-7 was found in nearly two-thirds of the cases, suggesting that this virus may be important for the development of angiosarcomas,” said Prof Chan.
Personalised treatments, better outcomes
With better understanding of angiosarcomas, scientists and doctors around the world can look to more targeted treatments to provide better patient outcomes.
For example, UV-related tumours are likely to respond to a type of treatment called immune checkpoint inhibitors, drugs that help white blood cells kill cancer cells. This form of treatment has also been shown to be promising for tumours with high mutation and inflammation scores in clusters one and three.
For patients in cluster two, scientists can explore using targeted therapies to fight tumour-promoting genes.
Currently, chemotherapy is the main form of conventional treatment for advanced angiosarcoma, said Prof Chan, but it is inadequate and many patients succumb within a year of diagnosis.
“We hope that immune checkpoint inhibitors will provide a more sustainable treatment response in patients with the appropriate tumour molecular profile, while avoiding the typical side effects from chemotherapy,” he added.
The team’s discovery is an inspiring breakthrough for doctors who are struggling to overcome challenges of managing angiosarcomas due to the severe lack of information.
"Understanding angiosarcomas will allow oncologists to treat their patients in a more targeted way. It is also a confirmation that NCCS is continuously conducting cutting-edge, translational research that has an impact on patients," said Professor Soo Khee Chee, senior author of the study and Founding Director, NCCS.
Eventually, the team hopes that this study will lead to a formal clinical trial that allows patients to be classified based on their angiosarcomas molecular profiles. “The discovery of clinically-actionable molecular targets in angiosarcoma and other rare cancers is expected to change the way we manage these patients,” said Prof Chan, whose team is planning to study other sarcoma subtypes.
Rare cancer isn’t all that rare
While investigators and funders have typically chosen to put their focus on common cancers, rare cancers as a collective actually account for a quarter of all cancer diagnoses.
The urgency for studying these little-understood diseases stems from the fact that rare cancers disproportionately affect adolescents and young adults, a group whose prognosis has not improved at the same rate as children and older cancer patients.
“The psychological uncertainties and physical burden of cancer on their personal life cannot be overstated,” said Prof Chan.
His research team started a new initiative called “STARLIGHT”, which aims to comprehensively investigate rare cancers. “We hope to increase the molecular understanding of rare cancers and eventually improve clinical outcomes of this group of diseases with unmet clinical needs,” Prof Chan explained.
At the same time, STARLIGHT will derive a precision-led treatment strategy. The strategy will guide personalised therapy and identify patients that are a good match for clinical trials. The establishment of the clinic also serves to promote scientific interest and collaboration among academic institutions and industry partners, eventually leading to innovation in the care of patients with rare cancers.
Get updates on Tomorrow's Medicine in your mailbox! Click here to subscribe.













 Get it on Google Play
Get it on Google Play