A mutated gene holds clues to nasopharyngeal cancer
A painless lump in the neck, a persistent sore throat, or frequent nose bleeds. These symptoms may seem innocuous but could be signs of nose cancer.
Nose cancer, or nasopharyngeal cancer (NPC), occurs deep in the nasal cavity – an area behind the nose and just above the back of the throat. Due to its location and non-specific symptoms, it is not easy to detect the disease in its earlier stages.
“In Singapore, 350 to 400 patients are diagnosed with nose cancer each year. About two-thirds of them are diagnosed with stage three or four nose cancers at the time of presentation,” said Dr Melvin Chua, Senior Consultant Radiation Oncologist at the National Cancer Centre Singapore (NCCS), which sees about 150 to 200 new nose cancer patients a year.
Nose cancer is prevalent in Southern China, Southeast Asia and Northern Africa. Locally, Chinese males between 40 to 60 years old, with or without a family history of nose cancer belong to the high-risk group.
Study revealed genetic link to NPC
An international key-opinion leader on nose cancer, Dr Chua co-led a large-scale collaborative study in Singapore, Hong Kong and China. The study brought together expertise from NCCS, which is at the forefront of nose cancer research, Sun Yat Sen Cancer Centre in Guangzhou – the world leading cancer institute in nose cancer, and the Chinese University of Hong Kong.
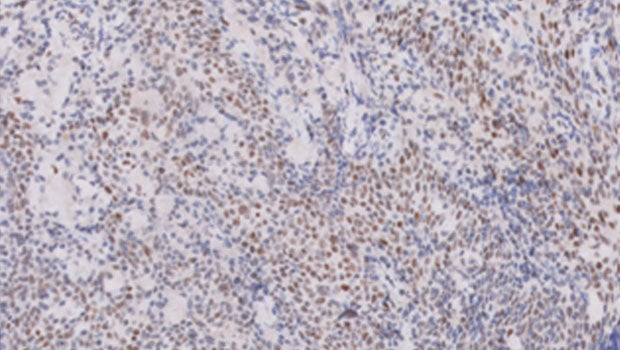
Spanning 5 years, the research team studied more than 5,000 nose cancer patients from the three institutions and discovered one gene – RPA1 that influence the survival of a patient following treatment (primary treatment is radiotherapy for nose cancer). The particular mutation of the RPA1 gene, known as rs1131636-T, is actually acquired by the individual at birth, and not only is it associated with nose cancer, but patients with this gene mutation may develop a more aggressive form of nose cancer that is resistant to radiotherapy.
This biomarker can thus be employed for screening, early detection, and most importantly, identify patients who are more likely to have aggressive nose cancer.
“There is potential to use the finding for screening among high-risk individuals. These patients can then be placed on active surveillance for early intervention if they develop this disease subsequently,” said Dr Chua, who is the co-first author of the study published in Advanced Science (Journal Impact Factor 15.804) in March 2020.
Potential treatment in the horizon
Distant metastasis (development of secondary malignant growths) is a major cause of treatment failures and poor survival in NPC. Currently, patients with stage one and two nose cancers are treated with radiotherapy alone, while patients in later stages may have concurrent chemotherapy and radiotherapy.
“For most nose cancer patients, radiotherapy is the primary treatmentbecause of the radiosensitive nature of its tumour cells and their position deep in the nasal cavity,” Dr Chua explained, “Therefore, tumours that are resistant to radiotherapy will recur and promote future metastatic seeding in the liver, lungs and bones.”
Another highlight from the study is the discovery of a regulator of the RPA1 gene – MiR-1253 gene. The team showed that the introduction of MiR-1253 can block the activity of RPA1. However, in nose cancer patients with the rs1131636-T mutation, the two genes are not able to bind together, causing this group of patients to have a more aggressive tumour. Understanding the interaction between Mir-1253 and RPA1 could pave the way to discovery of more potential therapeutic drugs for patients with resistant disease.
This international research collaboration proved fruitful to the clinician-scientists with the common goal of finding an effective biomarker for nose cancer. Not only was the team able to recruit a larger pool of patients collectively, it has produced findings that are clinically relevant, provocative and applicable across geographical regions.













 Get it on Google Play
Get it on Google Play