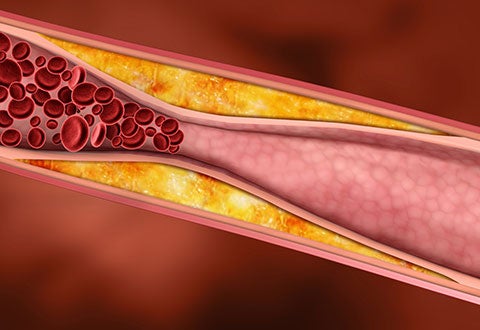
Coronary Interventions – a subspecialty that involves using non-surgical approach to treat narrowing of arteries of the heart found in coronary artery disease. (Photo: A close-up on narrowed artery)
By Dr Muhammad Bin Idu Jion, Consultant, Department of Cardiology, National Heart Centre Singapore
While many people with coronary artery disease can manage the disease with lifestyle changes and medications, others with severe conditions may need interventions such as coronary angioplasty to improve the health of the heart and blood vessels.
Cardiovascular disease encompasses ischaemic heart disease and cerebrovascular disease (stroke) and is a leading cause of mortality globally which accounts for up to 32% of all deaths. In Singapore, ischaemic heart disease is the third most common cause of death and hospitalisation.
Ischaemic heart disease occurs due to a build-up of plaque in the heart arteries (coronary artery disease), and the risk increases with age and presence of other chronic diseases such as diabetes, hypertension and dyslipidaemia (abnormal levels of lipids in blood), or other risk factors such as smoking, a sedentary lifestyle and a family history of myocardial infarction (heart attack).
Symptoms of ischaemic heart disease can present in several ways. Patients may present with an insidious onset of chest pain or breathlessness which occurs on exertion, termed stable angina, or they may present with heart failure signs and symptoms such as breathlessness on exertion or on lying flat, and water retention in the lungs and the lower limbs. Ischaemic heart disease can also present suddenly as an acute coronary syndrome, which range from unstable angina, nonST elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI). Acute coronary syndrome carries an average threemonth mortality rate of 5%. Patients with acute coronary syndrome may present with sudden or worsening chest pains and need to be hospitalised for treatment with medications such as antiplatelets, anticoagulants and statins, and undergo coronary evaluation and revascularisation if suitable. NHCS sees about 1,000 hospitalisations for acute coronary syndrome in a year that require coronary angiography for detecting narrowing in the arteries in the heart or angioplasty (minimally invasive, nonsurgical procedure for opening narrowed arteries).
Cases and Figures
On average, NHCS performs over 6,000 invasive cardiology procedures a year; of which majority of cases involve coronary intervention procedures. In 2018, 80% of the procedures were cases of coronary angioplasty and diagnostic coronary angiography (including left and right heart studies). Twenty percent were mainly non-coronary related procedures which included device-related procedures like permanent pacemaker insertions or implantable cardioverter defibrillators, electrophysiology studies and ablation cases, and structural heart (e.g. valvular or adult congenital) interventions.
Diagnostics and Treatment
With the advances in health screening and medical imaging technologies, coronary artery diseases can now be detected earlier through non-invasive imaging tests such as cardiac computed tomography (CT) calcium score and CT coronary angiogram, and non-invasive functional tests such as stress 2D echocardiogram, myocardial perfusion imaging and treadmill exercise stress. Newer non-invasive diagnostic tests like the stress cardiac magnetic resonance imaging (MRI) are also available in NHCS.
The mainstay of treatment for coronary artery disease is medical therapy with antiplatelets, statins, antianginals and risk factors control. However, invasive coronary assessment and therapies are usually required for acute coronary syndrome, symptomatic coronary artery disease and patients with severely abnormal non-invasive stress test results.

An overview of the cardiac lab procedures done in NHCS for 2018
Advances in Coronary Interventions
The median age of patients seen at NHCS outpatient clinics is approximately 60 years old. With an increasing older patient profile, challenging coronary anatomies with calcifications are frequently encountered during angioplasty. The prevalence of coronary calcification increases procedural complexity, duration and risks. Hence, NHCS continually improves coronary intervention technologies to better treat calcified and challenging coronary lesions. This includes bringing in the latest generation of drug eluting stents and maintaining a wide variety of coronary wires, balloons and micro-catheters.
For example, in addition to current cutting/ scoring balloons, which are used to pre-dilate calcified lesion, NHCS introduced the Non-Slip Element (NSE) lacrosse cutting balloon with nylon triangular cutting edges. This replaces the traditional wire cutting surface and helps reduce the risk of perforations. Another example is the procedure of atherectomy to debulk extensively calcified lesions prior to coronary stenting. In addition to the rotablator, which is a revolving instrument used to break up calcified plaque in a clogged coronary artery, NHCS acquired directional coronary atherectomy devices to facilitate the debulking of eccentric calcified lesions. There is also the addition of the coronary intravascular lithotripsy balloon catheter, where lithotripsy is a medical procedure that uses shock waves to break up hardened masses in the kidney, bladder, or ureter. Coronary lithotripsy is one of the latest procedures introduced in NHCS to deal with complex calcified coronary lesions.
While medical technology plays an important role in the diagnosis and treatment of coronary artery disease and ischaemic heart disease, it is vital to recognise that preventive measures such as lifestyle modifications and managing aggressive risk factors are essential and would definitely help improve patient outcomes.

A coronary angiography in progress.
This article is from Murmurs Issue 34 (May – Aug 2019). Click here to read the full issue.















 Get it on Google Play
Get it on Google Play