Complex congenital heart disease (CHD) encompasses a spectrum of congenital heart anomalies, requiring multidisciplinary management often throughout the patient’s lifetime.
Double outlet right ventricle (DORV) and ventricular septal defect (VSD)
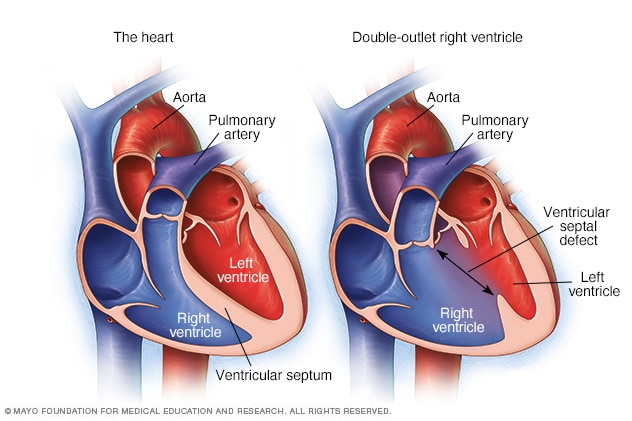
Figure 1. Comparison of a normal heart and a heart with double outlet right ventricle
Photo credit: MayoClinic.org Congenital heart defects in children Information
Double outlet right ventricle (DORV) describes a spectrum of congenital heart anomalies where the aorta and pulmonary artery arise from the right ventricle, in comparison to the structure of a normal heart where the aorta arises from the left ventricle. This rare condition occurs in about one per cent of patients with CHD1 resulting in the circulation of oxygen-poor blood in the body.
Anatomical adaptation with a ventricular septal defect (VSD) – a hole between the ventricles of the heart – which always occurs with DORV, allows oxygenated blood to flow from the left ventricle to the right side of the heart and enter systemic circulation.
Managing DORV – A joint venture of care
The management of DORV is greatly dependent on its type and association with other malformations that in turn determine the variable clinical manifestations of this condition. Owing to the complexity and numerous variations of this condition, challenges remain in determining the best treatment approach towards DORV.
Surgery has been the mainstay treatment approach for a majority of complex congenital heart diseases, including DORV. However, recent decades have seen a less invasive treatment approach2 powered by the unprecedented advancement of interventional techniques. The evolution of medicine and technology has further enabled interventional cardiology to palliate or even treat an increasing number of simpler cardiac diseases.3
These advances have propelled a joint venture of care involving cardiac surgeons and interventional cardiologists collaborating in the same setting2 – termed “hybrid procedure”– to harmoniously amalgamate invasive and less invasive treatment modalities to minimise risks and optimise treatment outcomes for patients.
Hybrid cardiac management for less invasive intervention
A hybrid cardiac procedure is defined as a treatment strategy that concomitantly adopts surgical and interventional approaches, and is done concurrently or sequentially within 24 hours.4 Less invasive hybrid procedures potentially allow for a reduction in cardiopulmonary bypass time and overall risks, and improved treatment outcomes for patients.5
Hybrid procedures have been an evolving area of clinical interest – the first trial took place in 1972, where a balloon catheter was used to temporarily occlude a patent ductus arteriosus (PDA) to allow for surgical closure from the inside.6 More recently, hybrid procedures have been adopted in the treatment of more complex conditions such as hypoplastic left heart syndrome (HLHS) and tetralogy of Fallot – all of which hinge upon the following fundamental indications: (i) intraoperative stent insertion into the pulmonary artery for relief of stenosis and (ii) balloon occlusion to control blood flow in between systemic to pulmonary circulation (e.g. PDA)8, (iii) PDA stenting and bilateral pulmonary artery banding (for HLHS)9.
Integration of both treatment modalities increases technical demands, necessitating intricate multidisciplinary teamwork. At KK Women’s and Children’s Hospital (KKH), patients with congenital heart diseases are benefiting from hybrid procedures administered by the dedicated, interdisciplinary paediatric cardiac care team. Established in 1997, the growing care team comprises experienced surgeons, cardiologists, cardiac-trained anaesthetists, intensivists and radiologists, who are committed to excellent and holistic care.
Case study: Hybrid cardiac management for a child with rare DORV and ventricular inversion Patient A was diagnosed at birth with DORV complicated by ventricular inversion and a large inlet VSD with severe pulmonary stenosis and hypoplastic pulmonary arteries. This caused his blood to flow from the morphologic right atrium into the morphologic left ventricle, through the VSD into the morphologic right ventricle, following the pulmonary arterial circulatory route to the left atrium, back to the morphologic right ventricle, before finally entering systemic circulation through the aorta. Drawing on hybrid cardiac management, the paediatric cardiac care team put together a complementary combination of surgical repair and interventional techniques to optimise treatment outcomes for patient A:
Patient A continues to undergo regular monitoring with continued multi-disciplinary management required as he transits into adulthood. Despite a paucity of data addressing hybrid procedures in the context of DORV in current literature, this demonstrates a first reported case of a paediatric patient in Singapore with DORV using a hybrid treatment modality, with a good treatment outcome thus far. |
This rare case is testament to the effective and complementary combination of surgical repair and interventional techniques in the treatment of complex CHD such as DORV. The treatment particularly for such an inherently complicated condition highlights the paramount importance of an individualised management strategy tailored to every patient’s different needs and variation of condition, to facilitate the best outcome possible. Tapping on the benefits of whilst combining both treatment modalities into a single therapeutic procedure would potentially lead to a paradigm shift in the treatment for complex CHD.
The Singapore healthcare system is underpinned by innovation, versatility and continual development of high quality healthcare with the current direction towards sophisticated healthcare. As the medical hub of the region, there is an increasing demand for state of the art medical technologies – giving it an edge in the integration of the hybrid approach into common clinical practice, further development of this modality and enhancement of global awareness. If employed effectively, this will pave the way towards increased survival rates and quality of life for children with complex CHD.
 |
Dr Nakao Masakazu obtained his medical degree from the Kyoto Prefectural University of Medicine, Japan. Completing his training in cardiothoracic surgery and paediatric cardiothoracic surgery in Singapore, Dr Nakao was awarded the Fellowship of the Royal Colleges of Surgeons for Cardiothoracic Surgery (FRCS-CTh) in 2011, and fulfilled his fellowship at Great Ormond Street Hospital for Children, London in 2013. Following his service as a consultant in paediatric cardiothoracic surgery at KKH, Dr Nakao was appointed the head of Heart Centre, Al Jalila Children’s Hospital, Dubai, in 2018. Dr Nakao is currently a senior consultant with the KKH paediatric Cardiothoracic Surgery Service since 2020. Dr Nakao’s interests are in the areas of congenital heart surgery, tracheal surgery, and translational research in congenital heart disease. Since 2010, he has been awarded several research grants from the SingHealth Foundation and National Medical Research Council. Dr Nakao’s career goal is to establish an international-standard unit for paediatric cardiology and paediatric cardiac surgery in Singapore. |
References:
|













 Get it on Google Play
Get it on Google Play