and hospital admissions with intensive treatment.
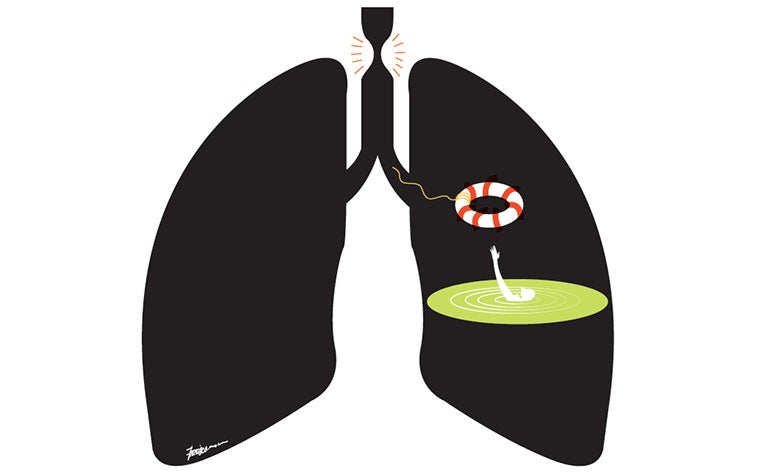
Whenever Ms S had a bad asthma attack, she would become so breathless that she wouldn’t be able to speak.
“I couldn’t get enough air in, I felt like I was drowning. I was afraid I might die because my aunt had died from asthma,” she told me.
Asthma patients experience coughing or wheezing, chest tightness and shortness of breath when their airways become inflamed and constricted because of cigarette smoke, air pollution, strong smells, allergies or respiratory tract infections.
While it’s possible to name the triggers, it’s less easy to pinpoint the causes. Both genetic and environmental factors are believed to be responsible – children whose parents have asthma have a greater tendency of developing it.
Exposure to cigarette smoke and viral infections during childhood are also possible causes.
Most children “outgrow” asthma but some with more persistent symptoms will continue to suffer from it well into adulthood.
About 20 per cent of children and 5 per cent of adults in Singapore suffer from asthma.
A common lung condition, it usually starts in childhood, although it can also appear for the first time in adults.
For most people, asthma can be controlled with regular use of medication. They are usually given two kinds of inhalers, known as controllers and relievers.
Controllers contain anti-inflammatory medications that are used daily. Relievers are used only when an asthma attack comes on. As the name suggests, relievers give quick relief from airway narrowing and are not substitutes for controllers as they do not have long-lasting action nor help to control the disease or prevent attacks.
Severe asthma, which affects 5 to 10 per cent of people with adult onset asthma, is harder to treat than mild or moderate asthma.
Such patients are likely to experience shortness of breath more than twice a week or have their sleep disrupted by attacks more than twice a month.
Even though they use high doses of controller medications, they still need relievers often, usually more than once a week because of frequent asthma attacks.
Ms S, who was 30 when she was diagnosed with asthma 15 years ago, belongs to this group who suffer from severe asthma symptoms.
She was seen at the Singapore General Hospital’s Severe Asthma Clinic, which typically receives about 200 patients a year.
New patients there will be assessed to see if the poor asthma control might be due to other conditions like allergies, gastrooesophageal reflux, obesity and obstructive sleep apnoea, or simply because they are not using their medication properly or regularly.
Based on the assessment, they will be given a treatment tailored to their individual needs and situation.
Many severe asthma patients – 75 per cent – do better in terms of a reduction in the number of severe attacks and hospital admissions after intensive treatment at the clinic. But about 25 per cent resist conventional treatment and may be offered other approaches like bronchial thermoplasty or injections known as biologics.
The injections help to block allergic responses or reduce the high levels of eosinophils – a type of white blood cell – to prevent severe asthma attacks, and improve asthma control and quality of life.
Three biologic drugs have been approved by the US Food and Drug Administration for severe asthma but many more are in development.
Bronchial thermoplasty, on the other hand, is a procedure which involves passing a scope into the lungs.
Heat waves are delivered to reduce the amount of muscle in the airways, which have thickened due to successive asthma attacks. This procedure helps make breathing easier.
Worldwide, close to 80 per cent of asthma patients who underwent bronchial thermoplasty saw improvement in their quality of life and made fewer emergency visits.
Ms S opted for bronchial thermoplasty six months ago and was pleased with the results.
“It does not cure asthma and I still need to use my controller inhalers daily, but I need to take less medication now. My asthma attacks are less frequent and I am less sensitive to smoke and strong smells,” she said.
“Most importantly, I can sleep better, take less medical leave from work and I can finally go overseas for a holiday.”
She used to have three or four severe attacks of asthma every year but has not had an attack since undergoing bronchial thermoplasty.
Associate Professor Mariko Koh is a senior consultant, department of respiratory and critical care medicine, and director of the Allergy Centre, Singapore General Hospital.
Contributed by














 Get it on Google Play
Get it on Google Play