Polyps in the colon can be detected and removed during regular colonoscopy.
Colonic polyps are mostly harmless. Some, however, can turn malignant and develop into colorectal cancer over time.
“That is why it is necessary to get a colonoscopy done every five to 10 years. Any polyp detected is then removed, whether it is malignant or not,” said Associate Professor Emile Tan, Senior Consultant and Head, Department of Colorectal Surgery, Singapore General Hospital (SGH).
Polyps are abnormal growths that appear in the colon (large intestines) or rectum. Healthy new cells in the bowel replace old ones on a daily basis. In some people, the new cells grow excessively, resulting in polyps forming. These can occur anywhere on the inner lining of the colon and are usually less than 1cm in diameter.
Most individuals have one to two polyps. But due to genetic conditions, some patients may have a “carpet of polyps”, where the number of polyps may go into the hundreds.
There are different types of polyps. Some, known as hyperplastic polyps, are merely overgrowths of normal cells and do not turn into cancer. “The most common type is called adenoma. While each adenoma has only a 1 per cent risk of becoming cancerous, nearly all malignant polyps start off as an adenoma,” said Assoc Prof Tan.
It takes a while before a polyp becomes cancerous, if at all. Assoc Prof Tan estimates that an adenoma takes about two to three years to grow 2 to 3cm in diameter, and another three to five years to transform into cancer.
“If the growth is faster than that, then we are dealing with a more aggressive cancer and prognosis will be much poorer. Generally, the bigger it grows, the higher the risk of it becoming cancerous,” he added.
Colonic polyps, even those up to 2cm in diameter, usually do not cause any symptoms and tend to be discovered only during routine colonoscopy screening. Patients with bigger polyps may experience symptoms, such as bloating or a change in bowel habit. If the polyp is in the rectum, there may be blood in the stools or a sensation of incomplete bowel emptying.
Once detected, the best treatment is a polypectomy, where the polyp is removed as completely as possible. This can be done during the colonoscopy. “It is important to remove polyps early, not only to prevent them from turning malignant, but also to ensure they do not grow too big because they can obstruct the bowel and affect its function,” said Assoc Prof Tan.
When the polyp is removed, it is sent to be assessed and graded for the level of dysplasia (cancerous change). High-grade dysplasia suggests mutations within the cells and a high chance of the polyp turning cancerous.
The level of dysplasia is a good indication of how regularly a colonoscopy should be done. If an individual has only one polyp of low-grade dysplasia, Prof Tan recommends a scope every three to five years. However, if there are more than five polyps, it is best to have a scope done every one to two years.
A polypectomy is, however, not an option when there are hundreds of polyps. As the condition has a genetic link, SGH tracks families with the condition through the Singapore Polyposis Registry. “These individuals undergo early screening and in some serious cases, they have prophylactic surgery done to remove the affected segment of the colon,” said Assoc Prof Tan. What you need to know about colonoscopy
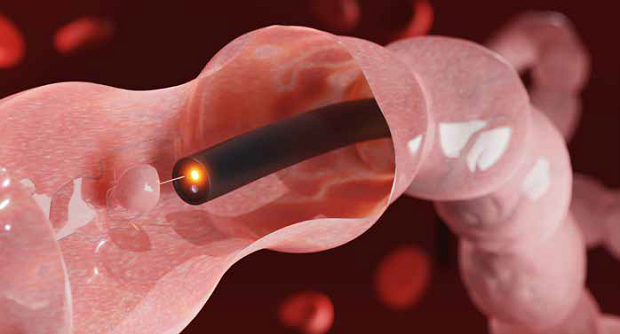
A colonoscopy allows the doctor to see the insides of your colon. Clearing the bowel thoroughly ensures an unobstructed view.
Before the scope
- Cut down on fibre intake about three to five days before the scope. Some foods and vegetables tend to stick to the colon, and this makes getting a good view of the insides difficult.
- Drink lots of fluids.
- Take strong laxatives with 2 litres of water the night before a colonoscopy to purge the remaining stools.
During the scope
- Colonoscopy is a day procedure done under sedation, and usually takes 30 to 40 minutes.
- A long, thin and flexible tube with a small camera attached (endoscope) is inserted into the colon through the anus.
Polyp removal
- The endoscope is able to lift the polyp, snare and remove it.
- Stalked polyps (long stalk, narrow base) are easier to detect and remove.
- Small and flat polyps are easier to miss and harder to remove. A solution is injected to the base to lift the polyp and aid removal.
- If a polyp is fixed to the base, has irregular borders or bleeds on contact, it is potentially cancerous.
- Titanium clips are used to close the base to prevent bleeding. These clips need not be removed and will eventually fall off spontaneously.
Who is at risk?
- About 15 per cent of people above 40 years old are likely to have colonic polyps. Other risk factors include:
- Aged 50 and above
- Chinese Genetic predisposition
- Relative with colorectal cancer before age 50
- Obesity
- Poorly controlled diabetes
- Excessive smoking or drinking
More frequent screening is recommended for these individuals.
Get the latest updates about Singapore Health in your mailbox! Click here to subscribe.













 Get it on Google Play
Get it on Google Play