Primary care physicians are often the first line of care for chronic obstructive pulmonary disease. Through the assessment of symptoms and risk of future exacerbations, patients can be stratified to aid in selection of initial treatment. By individualising treatment and making timely referrals to specialists, general practitioners are able to effectively diagnose and manage this long-term condition.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a common, preventable and treatable disease characterised by persistent respiratory symptoms and airflow limitation, usually due to cigarette smoking.1 The burden of COPD is staggering in Singapore, where it is the leading cause of respiratory disability and the tenth leading cause of death.2
COPD is a common condition that may present to primary care health providers, who play an essential role in diagnosing and managing this long-term condition.
CASE VIGNETTE
A 75-year-old man presents with exertional dyspnoea which has been progressive over the past year. He has to stop to catch his breath when traversing the distance between two bus stops. Almost daily, he has cough productive of whitish or yellowish sputum but this is not bothersome for him.
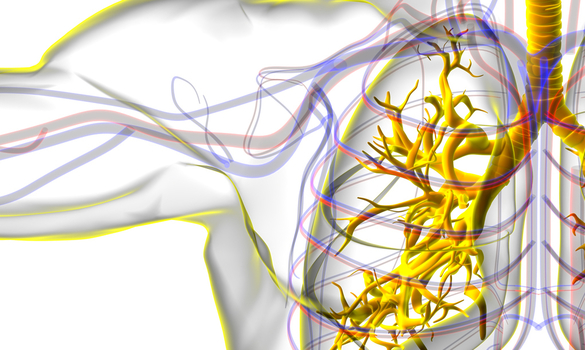
He has attended primary care once in the past year for a respiratory tract infection which required treatment with antibiotics. He has a 30 pack-year smoking history and is still actively smoking. Physical examination including vital signs is unremarkable. Chest x-ray is normal. Spirometry is shown in Figure 1. The COPD Assessment Test (CAT) score is 15.

Figure 1 Flow-volume loop with pre- and post-bronchodilator spirometry values
DIAGNOSING COPD
The patient described in the vignette is a smoker and demonstrates the chronic respiratory symptoms which are typical of COPD.
However, history and physical examination alone are not sufficient to make the diagnosis of COPD. Further investigations are needed to rule out other respiratory diseases that may present in a similar manner, as well as to confirm the diagnosis.
Chest x-ray is usually non-contributory in the diagnosis of COPD but is required to evaluate for
other diseases such as congestive heart failure,
tuberculosis, lung cancer and bronchiectasis. The confirmation of COPD requires spirometry testing. Specifically, the ratio of post-bronchodilator forced
expiratory volume in one second (FEV1) to forced vital capacity (FVC) should be less than 0.7.
The Global Initiative for Chronic Obstructive
Lung Disease GOLD Grade (1 to 4) is based on the
post-bronchodilator FEV1 % predicted, with lower
FEV1 % predicted values indicating a higher or more
advanced stage.
Whilst the GOLD grade predicts mortality and provides a useful gauge of the patient’s current status in the long-term disease trajectory, other patient-related outcomes are usually assessed during a consult to guide selection of initial pharmacologic treatment.
GUIDE TO SELECTING INITIAL TREATMENT
The two core patient-related outcomes of symptoms or impact and risk of exacerbation should be assessed at each visit.
1. Symptoms or impact
This can be assessed using either the modified Medical Research Council (mMRC) dyspnoea scale or the COPD assessment Test (CAT).
mMRC
mMRC is a simple scale measuring dyspnoea
when walking on level ground, ranging from 0
to 4 (Table 1), with mMRC scores of 2 or above indicating a higher symptom burden.
CAT
The CAT score quantifies the symptomatic impact
of COPD not only with respect to dyspnoea but
also other domains such as cough, mucous, chest
tightness, activities, sleep and energy. The CAT
score ranges from 0 to 40 with higher scores
indicating higher impact of symptoms. The patient
presented in the clinical vignette had a CAT score
of 15.
For the purpose of selecting initial treatment, a CAT score of 10 or more indicates a higher symptom burden.
Grade | Designation |
|---|---|
0 | Dyspnoea only with strenuous exercise |
1 | Dyspnoea when hurrying or walking up a slight hill |
2 | Walks slower than people of the same age because of dyspnoea or has to stop for breath when walking at own pace |
3 | Stops for breath after walking 100 yards (91 m) or after a few minutes |
4 | Too dyspnoeic to leave the house or breathless when dressing |
Table 1 Modified Medical Research Council (mMRC) dyspnoea scale
2. Risk of exacerbation
Whilst many factors may lead to an exacerbation, the strongest predictor for a future exacerbation is a history of previous exacerbation. The patient described in the vignette had experienced one exacerbation-like event which was treated as a respiratory tract infection by his primary care provider.
PHARMACOLOGICAL MANAGEMENT
Based on symptoms and risk of future exacerbations, patients can be stratified into different groups (ABCD) for initial treatment (Figure 2).
The patient in our vignette (one moderate exacerbation, CAT 15) falls under Group B, and may be commenced on a long-acting bronchodilator in the first instance, either a long-acting beta2-agonist (LABA) or long-acting muscarinic antagonist (LAMA).
Multiple inhaler devices are available for each class of medication, and the selection of inhaler device should be tailored to the individual patient to ensure that inhalers are used correctly. COPD outcomes are crucially dependent on delivering good basic care, and the adverse impact of inhaler misuse or nonadherence should not be underestimated.
Influenza and pneumococcal vaccinations are also recommended for COPD patients to reduce frequency and severity of infective exacerbations.
NON-PHARMACOLOGICAL MANAGEMENT
Non-pharmacological management of COPD is even
more important than pharmacological management.
Whilst pharmacological therapies have not been
found to have an impact on mortality, some non-pharmacological
interventions have a positive effect
on survival in COPD, chiefly smoking cessation, which
leads to slowing of the rate of lung function decline.
Even a few minutes invested on smoking cessation
counselling by physicians is associated with improved
quit rates among smokers.

LAMA: long-acting muscarinic antagonist; LABA: long-acting beta2-agonist; ICS: inhaled corticosteroids
WHEN REFERRAL IS NEEDEDWhere clinically indicated, GPs should refer COPD patients for specialist advice. Referral is appropriate at all stages of the disease, not only for those who are most disabled by the disease. Possible indications for GP referral include, but are not limited to:
Specialists can perform assessments for interventions such as:
COPD patients may also benefit from a range of hospital-based services including case management, social work, pulmonary rehabilitation, occupational therapy, dietetics, community care, and palliative care. Once stable, the care of COPD patients may be transferred back to primary care. |
CONCLUSION
In conclusion, COPD is a condition commonly encountered in primary care. The diagnosis of COPD should be confirmed on spirometry as far as possible. Combined assessment of symptoms (using either the mMRC or CAT score) and risk of future exacerbations (based on history of previous exacerbations) is used to stratify patients for the purpose of selecting initial treatment.
Referral for specialist advice is appropriate at all stages of disease, not only for those who are most disabled by the disease.
REFERENCES
-
Global Initiative for Chronic Obstructive Lung Disease (GOLD).
GOLD 2021 Global strategy for the diagnosis, management, and
prevention of chronic obstructive lung disease 2021 report. 2021.
- Epidemiology & Disease Control Division MoH, Singapore. Singapore Burden of Disease Study. 2010.
Dr Anthony Yii earned his medical degree from the University of Cambridge (UK) in 2009 and subsequently completed his specialty training in respiratory medicine in 2017. His scope of practice includes airway diseases (asthma, chronic obstructive pulmonary disease and bronchiectasis and pulmonary infections), interstitial lung disease, non-invasive ventilation, pleural diseases, diagnosis of lung cancer and bronchoscopy.
Apart from his clinical commitments, Dr Yii is active in pulmonology research with a focus on airway diseases and allergy and has been an invited reviewer for several international medical journals.
GPs can call the SingHealth Duke-NUS Lung Centre for appointments at the following hotlines, or scan the QR code for more information:
Singapore General Hospital: 6326 6060
Changi General Hospital: 6788 3003
Sengkang General Hospital: 6930 6000
KK Women’s and Children’s Hospital: 6692 2984
National Cancer Centre Singapore: 6436 8288













 Get it on Google Play
Get it on Google Play