By Dr Benjamin Ang, Consultant, Department of Orthopaedic Surgery, Singapore General Hospital
The article is contributed/written by Singapore General Hospital
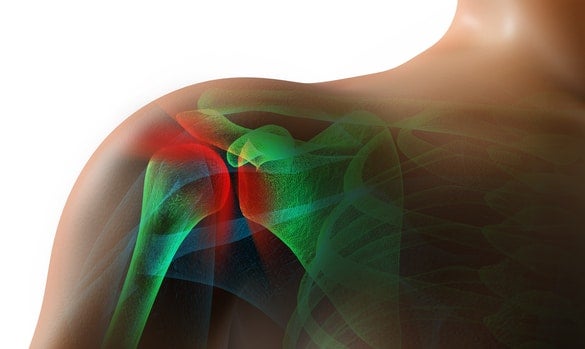
General practitioners are commonly presented with shoulder pain in their practice, where they are well-positioned to detect and administer first-line treatment for the underlying conditions. Read on for a review of common shoulder conditions and their management in primary care.
INTRODUCTION
Shoulder pain is a common presenting complaint seen in the primary care setting. Its causes may include:
- Frozen shoulder / adhesive capsulitis
- Rotator cuff tendinopathy
- Rotator cuff tear
- Subacromial impingement / bursitis
- Biceps tendinopathy
- Biceps tear
- Acromioclavicular joint (ACJ) osteoarthritis
- Glenohumeral joint osteoarthritis
- Cuff tear arthropathy
Frozen shoulder, or adhesive capsulitis, is the most common shoulder condition affecting middle-aged to elderly patients.
COMMON SHOULDER CONDITIONS
The upper limbs are frequently used in daily life, and any impairment due to pain and stiffness can limit activities of daily living, such as dressing or self-care, and may also result in difficulties with sleep or lying on the affected side.
The common presenting complaints, signs and symptoms during physical examination, and treatment options for the various common conditions are summarised in Table 1. Very often, a patient may have several co-existing conditions and thus present with a mixture of complaints, signs and symptoms.
It is important to exclude a cervicogenic source of pain by taking a history of neck pain, radiating pain down the forearm and numbness in the upper limb. It is also important to rule out non-orthopaedic differentials of shoulder pain, such as cardiac or gallbladder disease.
COMMON SHOULDER CONDITIONS | ||||
|---|---|---|---|---|
Condition | Presenting complaint | Signs and symptoms | Injections | Surgical intervention |
Frozen shoulder / adhesive capsulitis | Shoulder pain and/or stiffness | Limited active and passive range of motion | Glenohumeral joint H&L and hydrodilation | Arthroscopic capsular release and manipulation under anaesthesia |
Rotator cuff tendinopathy, rotator cuff tear | Shoulder pain and/or weakness | Weakness, painful arc, drop arm sign positive | Not recommended for rotator cuff tear | Arthroscopic rotator cuff debridement/repair/augmentation |
Subacromial impingement / bursitis | Shoulder pain in certain positions | Hawkins-Kennedy test positive, Neer’s test positive | Subacromial H&L | Arthroscopic subacromial decompression, bursectomy, acromioplasty |
Biceps tendinopathy, biceps tear | Shoulder pain over bicipital groove | Bicipital groove tenderness, Speed’s test positive, Yergason’s test positive, Popeye sign if complete tear | Bicipital groove H&L | Arthroscopic biceps tenotomy or tenodesis |
Acromioclavicular joint (ACJ) osteoarthritis | Shoulder pain over ACJ | ACJ tenderness, cross-body adduction test positive | Acromioclavicular joint H&L | Arthroscopic excision of distal clavicle |
Glenohumeral joint osteoarthritis | Shoulder pain and/or stiffness | Limited active and passive range of motion | - | Total shoulder arthroplasty |
Cuff tear arthropathy | Shoulder pain and/or weakness | Weakness, painful arc, drop arm sign positive | - | Reverse shoulder arthroplasty |
Table 1 Common shoulder conditions and their presenting complaints, signs and symptoms and treatment options
H&L: Hydrocortisone and lignocaine
INVESTIGATIONS FOR COMMON SHOULDER INJURIES
X-rays, ultrasounds and magnetic resonance imaging (MRI) scans are the commonly performed investigations for shoulder pain work-up.
X-rays
In the context of trauma, basic X-rays are required to rule out fractures and dislocations. X-rays are recommended to rule out glenohumeral joint arthritis when diagnosing frozen shoulder. It can also serve as a baseline investigation and pick up acromioclavicular joint arthritis and subacromial spurs.
Ultrasounds
An ultrasound of the shoulder is useful to look for other concomitant conditions such as rotator cuff tears, subacromial bursitis and biceps tendinopathy. However, it is unable to pick up intra-articular lesions such as labral tears.
MRI
MRI is the most advanced imaging technique and also the most expensive. It allows for assessment of all the above conditions, and is the preferred mode of imaging for preoperative planning.
MANAGING COMMON SHOULDER INJURIES
Diabetes screening
For patients with frozen shoulder, screening for diabetes mellitus is recommended in view of the high correlation between the two conditions.
Oral analgesia and lifestyle modifications
In the primary care setting, oral analgesia such as paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) should be prescribed for pain relief. Topical NSAIDs may also be prescribed for more targeted local effect.
Inflammation from bursitis and arthritis may be improved from the use of NSAIDs. Advice for lifestyle modification may also be beneficial.
Physiotherapy
For most shoulder conditions, a trial of physiotherapy for at least a few months is recommended. Physiotherapy exercises can help improve shoulder range of motion and muscle strength, to help patients improve their abilities to perform daily activities.
Surgery
If the symptoms are severe and debilitating, and after failure of conservative management, different surgical options as detailed in Table 1 may be considered. Surgery is usually performed arthroscopically using a few keyhole incisions, except for arthroplasty ( joint replacement) which requires an open approach.
The choice of procedures required will be individualised to the patient’s signs, symptoms and underlying condition(s), with the appropriate procedures performed to address each individual pathology.
Surgery is also the only way to repair a torn rotator cuff. The other treatments mentioned above will not ‘cure’ it, but may help alleviate the patient’s symptoms. For young patients with an acute, traumatic rotator cuff tear, early surgery is recommended. Otherwise, a trial of physiotherapy is preferred.
However, in certain cases of unrepaired rotator cuff tear, there is a risk of progression of the size of rotator cuff tear, and subsequently to end-stage cuff tear arthropathy.
SHOULDER DISLOCATION
In the younger population, shoulder dislocation is the most common shoulder complaint. Traumatic shoulder injuries may occur at any age, and are commonly associated with labral tears in young patients and rotator cuff tears in older patients.
Anterior dislocation is the most common direction of shoulder dislocation. It is usually a result of trauma, although recurrent dislocation may also be atraumatic. Posterior dislocation may be the result of electrocution or seizures.
Diagnosis
Clinically, painful range of motion and squaring of the shoulders is suspicious for dislocation.
X-rays, particularly axial or Velpeau views, are useful to diagnose dislocation, and to confirm enlocation after manipulation and reduction.
After reduction, MRI is the investigation of choice as it can pick up labral tears, Hill-Sachs lesions, and other intra-articular pathologies. For an elderly patient who suffers a dislocation, a rotator cuff tear is not uncommon and can be picked up on MRI as well.
With recurrent dislocations, there may be anterior glenoid bone loss or a large Hill-Sachs lesion. Occasionally, a computed tomography (CT) scan may be required for better assessment of the bony defect for surgical planning.
Management
Acute management of a dislocated shoulder involves manipulation and reduction under sedation. This is commonly done in the emergency department. After reduction, an arm sling may be used for support and to immobilise temporarily until the pain resolves.
The recommended treatment for recurrent shoulder dislocation is surgery. This may include labral repair, capsular plication, remplissage and/or bone block procedures. At the time of surgery, other concomitant pathologies may also be addressed.
Physiotherapy for strengthening of the rotator cuff muscles is also a crucial adjunct to prevent recurrence.
CONCLUSION
Analgesia, lifestyle modifications and physiotherapy are the first-line treatment for most shoulder conditions. Injections may be a useful adjunct in certain conditions. Surgical intervention should be considered after failure of conservative management. Surgery is the recommended initial treatment in certain cases, such as for young patients with an acute traumatic rotator cuff tear and for patients with recurrent shoulder dislocations.
THE DEPARTMENT OF ORTHOPAEDIC SURGERY AT SINGAPORE GENERAL HOSPITAL |
|---|
| Singapore General Hospital’s Department of Orthopaedic Surgery performs an average of over 400 shoulder surgeries per year. The department’s Sports Service does a large majority of these surgeries, including arthroscopic surgeries and open surgeries for arthroplasty – addressing all the above-mentioned conditions and others such as fractures. |
Dr Benjamin Ang is an Orthopaedic Surgeon with the Department of Orthopaedic Surgery in Singapore General Hospital. He is an avid sportsman and has previously represented Singapore at international competitions in track & field and floorball. With first-hand experience and a personal understanding of an athlete’s psyche, he sub-specialises in sports orthopaedics. His interests lie in managing shoulder, hip and knee conditions. He was awarded the Ministry of Health HMDP (Health Manpower Development Plan) award for further fellowship training in hip surgery in Switzerland.
GPs who would like more information about these conditions and procedures may contact Dr Ang at benjamin.ang.f.h@singhealth.com.sg.
GP Appointment Hotline: 6326 6060
GPs can visit the website for more information about the department.













 Get it on Google Play
Get it on Google Play