Primary care physicians are often the first to see patients who suspect they have cancer, heart disease, neurological disorders and more. While the care of these patients is usually referred to specialists, general practitioners may find it useful to discover how cell therapy may now be employed to treat complex diseases in some cases when conventional treatment does not work.
WHAT IS CELL THERAPY?
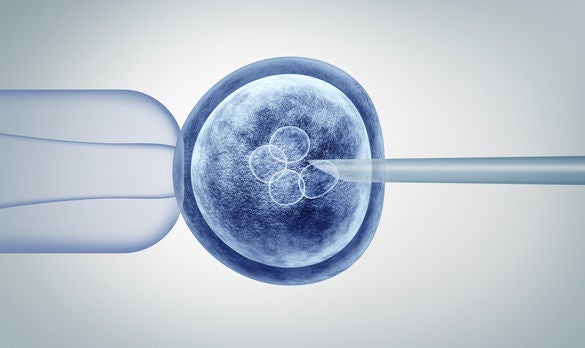
Cell therapy is an exciting new field of medicine, where cells are used as living drugs that will continue to grow in the patient to exert and amplify their beneficial effects for the long term. This has been a big revolution in medicine and many patients around the world have been benefitting from the use of cells for treatment.
There are two main categories of cell therapy: cellular immunotherapy and regenerative medicine.
In cellular immunotherapy, immune cells are grown and 'trained' to fight diseases like cancer and infectious diseases by resetting the immune system and/or through genetic modifications of the immune cells.
Cellular regenerative medicine is a fast-growing area of medicine that restores, repairs or replaces damaged cells, tissue or organs in the body. This is particularly relevant for progressive disease conditions such as heart disease, eye degeneration, and neurological and musculoskeletal disorders.
WHAT CONDITIONS CAN BE TREATED WITH CELL THERAPY?
The use of cell therapy is growing and diversifying. Several new cell therapy products have been approved by the United States Food and Drug Administration (FDA) in recent years, with more to come.
Haematological conditions
The chimeric antigen receptor T cell (CAR T cell) is one such example. These are patient-derived T cells that undergo genetic modification to express an artificial T cell receptor against an antigen that is expressed on the surface of cancer cells.
Currently, there are five FDA-approved CAR T cells for use in haematological conditions such as:
- Acute B-cell lymphoblastic leukaemia (ALL)
- Diffuse large B-cell lymphoma (DLBCL)
- Mantle cell lymphoma (MCL)
- Multiple myeloma (MM)
Patients must have received at least two lines of treatment and not responded before they can receive CAR T-cell therapy.
Age-related diseases and chronic conditions
Cellular regenerative medicine has been applied in the treatment of age-related diseases and chronic conditions, for example:
- Regenerated blood cells are used to treat bone marrow and blood disorders of the bone marrow
- Stem cells are used to treat eye diseases like corneal disease
- Regenerated skin cells are used for acute and chronic wound healing like burns
Other applications
In 2016, the FDA approved the use of an autologous cellularised scaffold product for the repair of symptomatic cartilage defects of the knee.
Regenerative medicine cell therapy applications are also being studied for future clinical use in heart disease, muscle wasting, and diseases like Parkinson and Alzheimer's.
WHO IS ELIGIBLE FOR CAR T-CELL THERAPY IN SINGAPORE?
Singapore General Hospital was the first site in Southeast Asia to be approved for the FDA-registered CAR T-cell therapy for ALL and DLBCL. Many of its patients receiving CAR T-cell therapy have attained control of leukaemia and lymphoma, when they were previously resistant to all forms of chemotherapy.
| Current indications | Upcoming indications | Potential future indications (in development) |
|---|---|---|
|
|
|
BUILDING A PIPELINE OF CELLULAR AND REGENERATIVE THERAPIESLaunched earlier this year in May 2021, the SingHealth Duke-NUS Cell Therapy Centre (SDCT) will prepare clinical teams for the cell therapy revolution. Launched concurrently with SDCT is the SingHealth Duke-NUS Regenerative Medicine Institute of Singapore (REMEDIS), which will harness the potential of regenerating diseased cells, tissue and even organs to tackle age-related diseases and chronic conditions. The establishment of REMEDIS and SDCT sets up a bench-to-bedside pipeline – REMEDIS will develop research, regenerative therapies and tools, while SDCT will bring the treatments directly to patients by taking these into clinical trials and clinical applications that can benefit patients. SDCT will also focus on training and enabling clinical teams to bring to patients the best that cell therapy has to offer. |
FUTURE APPLICATIONS ON THE SINGHEALTH CAMPUS
Applying cell therapy to overcome limitations in existing treatment options
With support from the National Research Foundation Singapore, applications of cellular regenerative medicine on the SingHealth campus will kick off with a research study led by clinician-scientists from the SingHealth Duke-NUS Academic Medical Centre.
Professor William Hwang, Medical Director of the National Cancer Centre Singapore and Lead Principal Investigator of the study, with Team Principal Investigators Professor Karl Tryggvason and Assistant Professor Tay Hwee Goon from the Cardiovascular and Metabolic Disorders Programme at Duke-NUS Medical School, will develop cellular therapy products for three disease areas:
- Age-related macular degeneration
- Ischaemic cardiomyopathy
- Blood cancers
Due to the limitations of existing therapies, the research team is working towards safe and effective treatments for patients affected by these conditions.
Developing stem cells for regenerative medicine
Professor Tryggvason, a world-renowned researcher from Duke-NUS, is a leader in laminin technology. Laminins form the basement membrane on which cells grow in many tissues and, in tissue culture, they give a road map to cells to tell them what kind of cells they should become.
His team has been able to produce exciting functioning cells that seem to work in animals to repair cells of the heart, eye and skin. The research team intends to enhance this process with small molecules and to extend the use of these laminins for bone marrow diseases.
If the development of cellular therapy products and pre-clinical models is successful, the team has plans to conduct clinical trials and commercialise the products. In addition, the team will document and chart the process and development of the products with scientific studies and patents, which will add to knowledge about regenerative medicine that can ultimately be used in biomedical and clinical applications to improve patient care.
ADVISING PATIENTS ABOUT CELL THERAPY
Not all activities in cell therapy and regenerative medicine are based on solid science, and we need to be responsible gatekeepers to only adopt those which have good clinical and pre-clinical evidence.
A lot of this work is still in the research phase and not yet in clinics, but cell therapy is fast becoming a viable treatment option and no longer science fiction.
THE ROAD AHEAD
In Singapore, there is growing interest in cell-and-tissue-based products as potential treatments for a variety of diseases. The government has taken measures to advance cell therapy through the establishment of a local Good Manufacturing Practice (GMP) facility, the Advanced Cell Therapy and Research Institute, Singapore (ACTRIS), and investing $80 million of national funds in cell therapy research.
The recently implemented local regulatory framework for cell, tissue and gene therapy products (CTGTP) is another measure to allow the use of these therapies in Singapore with guidance.
Medical professionals who would like more information about the available cell therapies, please direct your enquiries to sd.cell.therapy@singhealth.com.sg.
Professor William Hwang is the Medical Director of the National Cancer Centre Singapore, Head of the SingHealth Duke-NUS Cell Therapy Centre, Chair of the Oncology Academic Clinical Programme at Duke-NUS Medical School and Senior Consultant at the Department of Haematology, Singapore General Hospital. He is also an Executive Board Member of the Asia-Pacific Blood and Marrow Transplantation Group, as well as Board Organising Committee Member of the Singapore Translational Cancer Consortium and Advanced Cell Therapy Research Institute of Singapore.
Assistant Professor Francesca Lim is a Consultant Haematologist at Singapore General Hospital (SGH), Deputy Head and Principal Lead (Education) at the SingHealth Duke-NUS Cell Therapy Centre and Assistant Medical Director at the Cell Therapy Facility, Health Sciences Authority. She spent two years training at the MD Anderson Cancer Center in CAR T-cell therapy, particularly in CAR-NK cell therapy. She has been instrumental in supporting and coordinating the Cell Therapy Programme at the SGH Department of Haematology, both at the clinical and research levels.
GPs can contact the SingHealth Duke-NUS Cell Therapy Centre at sd.cell.therapy@singhealth.com.sg to know more about the available cell therapies and clinical trials on the SingHealth campus.













 Get it on Google Play
Get it on Google Play