1. Non-invasive Treatment: SGH pioneers MR-guided ultrasound for prostate cancer, promising effective tumor destruction without damaging healthy tissue, unlike conventional methods like surgery or radiation.
2. Minimized Side Effects: Unlike traditional treatments, which often cause incontinence and impotence, this new procedure aims to preserve quality of life for patients with early-stage prostate cancer.
3. Precision and Safety: Using precise MR guidance, the procedure targets tumors as small as a millimeter, ensuring minimal complications and potentially preserving normal urinary and sexual function for patients.
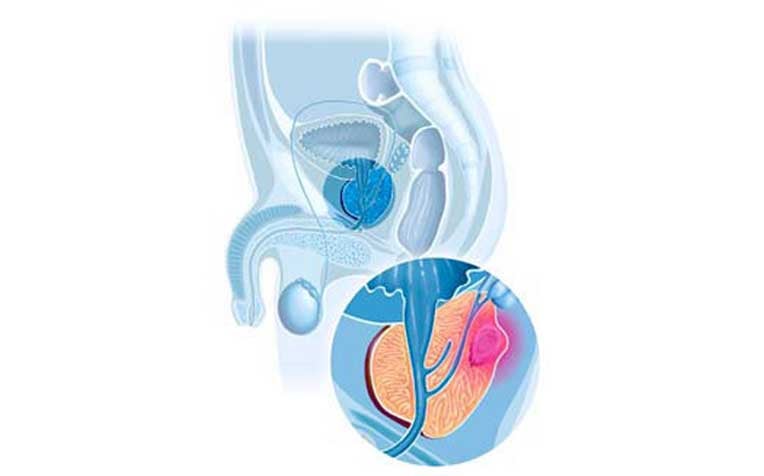
Common side effects of prostate treatment include incontinence and impotence. A non-invasive method of prostate cancer treatment can minimise the side effects caused by damage to the functional areas of the prostate.
SGH pioneers new non-invasive treatment for prostate cancer
Prostate cancer is occurring four times more frequently compared to 30 years ago, and about four in 100 men diagnosed with the disease die from it. As Singapore’s population rapidly ages, this trend is expected to speed up. While tests are able to pick up the disease at a much earlier stage, treatment can leave a man feeling less of a man.
Conventional treatments for cancer of the prostate – the gland that forms part of the male reproductive system – include the surgical removal of the prostate gland (prostatectomy), radiation therapy, implantation of radioactive seeds (brachytherapy) and using low temperature to impede cancer cell metabolism (cryotherapy).
“Unfortunately, current treatments are accompanied by lasting side effects which significantly impact the quality of life of prostate cancer patients,” said Professor Christopher Cheng, Senior Consultant, Urology Centre, Singapore General Hospital (SGH), a member of the SingHealth group.
“The most common are incontinence and impotence."
But a clinical trial at SGH, in collaboration with the National Cancer Centre Singapore (NCCS), could soon offer men with early stage, low-risk prostate cancer a cure, without the drawbacks.
This procedure uses magnetic resonance (MR)-guided ultrasound – the same technology used to treat uterine fibroids in women – to help surgeons locate the tumour and surrounding tissues precisely, and focus the pulses of sound waves to “burn” the tumour. Known as MR-guided focused ultrasound treatment for prostate cancer, the procedure doesn’t damage nearby healthy tissue.
Up to March 2011, 18 patients aged between 50 and 75 years, with localised low-risk prostate cancer, have been treated as part of this international multicentre clinical trial, the first of its kind in the world. With seven patients treated here so far, Singapore is the largest centre for this trial.
According to Prof Cheng, the non-invasive method is able to provide effective treatment while minimising the debilitating side effects caused by damage to the functional areas of the prostate, surrounding organs and structures. But it also addresses another patient concern.
“With prostate cancer being diagnosed earlier, this is an important development because at present, we are very mindful about over-treating some patients with a prostatectomy or radiation therapy, for instance.
“On the other hand, if we choose a less aggressive approach – active surveillance, maybe repeating certain tests or doing another biopsy – patients may feel that nothing is being done to directly treat their condition. So this can serve as a middle-ground solution, especially for the older age group with early stage prostate cancer,” said Prof Cheng.
How the procedure works
Performed as a day procedure at NCCS, the treatment involves inserting a transducer – a device to transform one form of energy to another – into the rectum of the patient, who lies on his back with his legs elevated. No incisions are required.
“With MR guidance, hundreds of individual and normally harmless sound waves are directed at a single treatment point deep inside the body. When they intersect, these ultrasound waves have enough energy to destroy tumour cells,” said Dr James Khoo, Senior Consultant and Head, Department of Oncologic Imaging, National Cancer Centre Singapore (NCCS), a member of the SingHealth group.
The concept, Dr Khoo added, is similar to the way that rays of sunlight can be focused through a magnifying glass to start a fire, or burn a hole in a piece of paper.
“The technology is so precise that it can treat sites as small as a millimetre, which is about the size of half a grain of rice,” he said.
During the procedure, tools such as real-time MR thermometry and a 3D accumulated dose display, help monitor and control heat distribution, as well as mark the boundaries of the tumour to be burned.
Given the precision involved, it is not surprising that the patient has to stay absolutely still during the treatment. He may be given a spinal epidural or put under general anaesthesia to ensure minimal or no movement. The procedure can take about three hours on average to complete.
Since the trial started in August 2010, other than occasional difficulty when urinating, patients have not experienced any major complications. Neither have there been any relapses, the doctors said.
“Hopefully, when this becomes a standard method of care, more men with early prostate cancer will get treated with it and return to having a satisfying sex life,” said Prof Cheng.
What is the prostate?
The prostate, which forms part of the male reproductive system, is a walnut-sized gland located in front of the rectum and just below the bladder. It wraps around the urethra, the tube carrying urine from the bladder through the penis.
The prostate requires mainly testosterone (the male hormone) to function properly. One of its functions is to produce fluid for semen to transport sperm during ejaculation. When prostate cells grow abnormally, the organ enlarges and pushes against the urethra and bladder, blocking the normal flow of urine.
Cancer that begins in the prostate may remain in the prostate or spread to nearby lymph nodes. In some cases, it can even spread to the bones, bladder, rectum and other organs.
Screening for prostate cancer is important, since the disease rarely shows any definitive signs in the early stages. As the disease progresses, however, prostate cancer patients may find themselves having to urinate more frequently and urgently, but with less urine or even blood in the urine.
Ref: N18
Contributed by

















