Delayed diagnosis contributes to the poorer prognosis of rare cancers such as sarcomas. The National Cancer Centre Singapore shares how GPs are key to early detection and referral, for better patient outcomes.
INTRODUCTION
Sarcomas are a heterogeneous group of rare malignant tumours, making up less than 1% of all adult and around 21% of paediatric solid cancers.1
They are mesenchymal in origin and arise virtually anywhere in the body, from both skeletal as well as soft tissue, including that of muscle, fat, joints and blood vessels, and fibrous connective tissue. In terms of body distribution of these soft tissue sarcomas, approximately 40% occur in the extremities, 38% in the abdomen and 10% in the trunk.2
CLINICAL PRESENTATION
Presentation can be vague and non-specific depending on the anatomic location, and therefore a high index of suspicion is necessary.
It is not uncommon for them to be mistaken for benign soft tissue masses such as lipomas, given the fact that they outnumber malignant lesions by 100:1, and most primary care practitioners will only encounter one to two cases in their decades of practice.3
Nevertheless, the majority of lumps eventually diagnosed as sarcomas first present in the primary care setting, and the role that general practitioners (GPs) play in the early detection of sarcomas cannot be understated.4
IMPORTANCE OF EARLY DETECTION AND DIAGNOSIS
Due to their rarity, experience in terms of recognition, workup, as well as subsequent management outside of tertiary specialist centres currently remains suboptimal. Patients with rare cancers such as sarcomas suffer from a comparatively poorer prognosis than common cancers, with a delay in diagnosis being a major contributor to this outcome.5
Importantly, early detection and diagnosis allow for less extensive and morbid surgeries and are associated with improved patient outcomes.6-8
In line with this, national frameworks and guidelines have been implemented in many countries around the world to facilitate fast-track referrals of suspected sarcoma cases that present in the primary care setting, such as the ‘two-week wait’ pathway outlined by the National Institute for Health and Care Excellence in the United Kingdom9.
THE SPEED INITIATIVE AT THE NATIONAL CANCER CENTRE SINGAPORE
The Department of Sarcoma, Peritoneal and Rare Tumours (SPRinT) at the National Cancer Centre Singapore (NCCS) comprises a team of surgical oncologists trained in the complex management of sarcomas, in collaboration with multidisciplinary experts from various sub-specialties.
In Singapore, SPRinT has established the SPEED (Sarcoma Pre-Emptive Evaluation and Diagnosis) initiative to fast-track early diagnosis of sarcomas in order to improve patient outcomes.
Under this initiative, the department welcomes all referrals, including from GPs, of lumps suspicious for sarcoma without a need for prior imaging.
Referral criteria
The referral criteria include the presence of any one of the following features, easily remembered by the mnemonic ‘5 FOES’:
- >5 cm in size
- Deep to Fascia
- Ouch (painful)
- Enlarging
- Stuck to surrounding structures

Figure 1 The SPEED initiative (click to expand infographic)
OPTIMISING OUTCOMES WITH MULTIDISCIPLINARY CARE
The diagnostic workup and management of soft tissue sarcomas are complex. It encompasses accurate clinical assessment supported by appropriate radiological and histological investigations as well as molecular diagnostics. This is accompanied by the ready availability of multimodality treatment options, most commonly involving some combination of chemotherapy, radiotherapy and surgery, plus the support of allied health and ancillary services such as therapists, medical social workers and case managers.
All sarcoma cases at NCCS are reviewed at a weekly multidisciplinary tumour board and managed holistically. It has been demonstrated that this level of coordinated service translates to improved outcomes for patients, and is best achieved at tertiary high-volume centres.10,11
Within SingHealth, the surgical management of sarcoma cases is spearheaded by SPRinT, in collaboration with the various surgical disciplines including that of plastic, reconstructive and aesthetic surgery, orthopaedic surgery, vascular surgery as well as urology. Outcomes have been found to be comparable to other international high-volume centres.12
Presentation
Mr M is a 62-year-old who presented to SPRinT with a left flank mass that had been progressively enlarging for six months. Its presence was associated with a loss of appetite and weight, as well as back pain. Diagnostic investigations
Investigations revealed the presence of a large infiltrative dedifferentiated liposarcoma arising from the left retroperitoneum, with involvement of the lower chest wall, lateral thoracoabdominal wall, left kidney, tail of pancreas, spleen and segments of the descending colon.
Treatment and outcomes
His case was discussed at a multidisciplinary tumour board, which recommended a plan for treatment with surgery and radiotherapy.
Mr M underwent wide excision of the mass with resection of the left lower ribs and diaphragm, left nephrectomy, distal pancreatectomy and splenectomy, as well as limited left hemicolectomy, with reconstruction of the surgical defect using a pedicled anterolateral thigh flap.
Postoperatively, he recovered well and went on to complete treatment with adjuvant radiotherapy. He is currently well with no evidence of disease recurrence and continues to be on regular follow-up with us for surveillance.
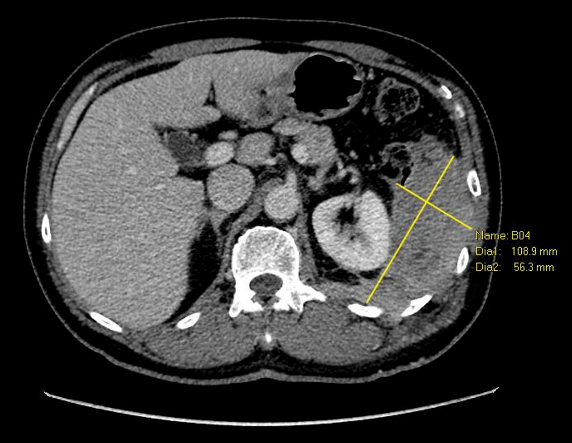 Figure 2 Preoperative scan showing dedifferentiated liposarcoma requiring multivisceral resection
 Figure 3 Postoperative photo showing complete resection and good recovery with abdominal wall reconstruction, with the help of a multidisciplinary team |
THE SPRinT SERIES: PARTNERING GPs TO CARE FOR ADVANCED AND RARE CANCERS
This is the second in a five-part series of articles, ‘The SPRinT Series’ – in which we discuss the work that SPRinT does, the key aspects of SPRinT’s clinical focus and the role of general practitioners (GPs) in providing care.
Due to the rarity of these tumours, it is critical for patients to be promptly referred to a specialist department/centre, such as SPRinT, to provide the best outcomes.
GPs are our first line of defence, and close collaboration between SPRinT and the GP community is essential for the timely diagnosis and referral of patients with rare tumours.
Read part one of the series here:
Partnering GPs to Care for Advanced and Rare Cancers
For GP referrals to the Department of Sarcoma, Peritoneal and Rare Tumours (SPRinT), please contact NCCS at:
Hotline: 6436 8288
Email: [email protected]
Click here for more information on the department. |
REFERENCES
Burningham, Z., et al., The epidemiology of sarcoma. Clin Sarcoma Res, 2012. 2(1): p. 14.
Brennan, M.F., et al., Lessons learned from the study of 10,000 patients with soft tissue sarcoma. Ann Surg, 2014. 260(3): p. 416-21; discussion 421-2.
Mannan, K. and T.W. Briggs, Soft tissue tumours of the extremities. BMJ, 2005. 331(7517): p. 590.
Buvarp Dyrop, H., et al., Routes to Diagnosis for Suspected Sarcoma: The Impact of Symptoms and Clinical Findings on the Diagnostic Process. Sarcoma, 2016. 2016: p. 8639272.
Blay, J.Y., et al., The value of research collaborations and consortia in rare cancers. Lancet Oncol, 2016. 17(2): p. e62-e69.
Ferrari, A., et al., The symptom interval in children and adolescents with soft tissue sarcomas. Cancer, 2010. 116(1): p. 177-83.
Grimer, R.J., Size matters for sarcomas! Ann R Coll Surg Engl, 2006. 88(6): p. 519-24.
Nakamura, T., et al., The symptom-to-diagnosis delay in soft tissue sarcoma influence the overall survival and the development of distant metastasis. J Surg Oncol, 2011. 104(7): p. 771-5.
Suspected cancer: recognition and referral NICE guideline NG12, Section 1.11. 2015, National Institute for Health and Care Excellence.
Lazarides, A.L., et al., Soft Tissue Sarcoma of the Extremities: What Is the Value of Treating at High-volume Centers? Clin Orthop Relat Res, 2019. 477(4): p. 718-727.
Blay, J.Y., et al., Improved survival using specialized multidisciplinary board in sarcoma patients. Ann Oncol, 2017. 28(11): p. 2852-2859.
Tu, I.W., et al., Department of Sarcoma, Peritoneal and Rare Tumors (SPRinT): A subspecialty surgical oncological care model for advanced malignancies requiring complex procedures. Asian J Surg, 2022. 45(1): p. 546-548.
